Chronic Kidney Disease Diet: What to Eat, Avoid, and Why It Matters
When your kidneys aren’t working right, what you eat becomes just as important as any pill you take. Chronic kidney disease diet, a personalized eating plan designed to reduce the workload on damaged kidneys and prevent dangerous buildups of waste, minerals, and fluids. Also known as renal diet, it’s not about starving or cutting out everything you love—it’s about making smarter choices so your body doesn’t have to work overtime just to stay balanced. If you’re managing chronic kidney disease, a long-term condition where kidneys slowly lose their ability to filter blood, your diet helps control blood pressure, stop fluid swelling, and delay the need for dialysis.
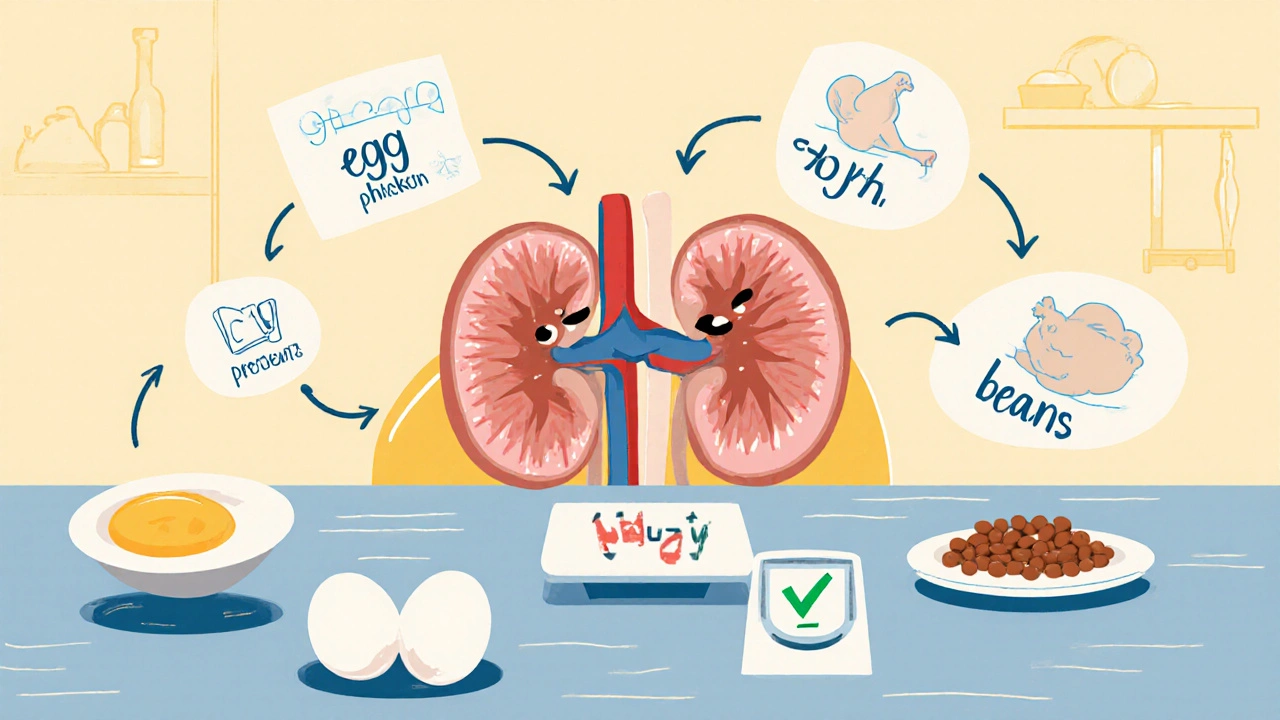
Three big players rule this diet: sodium, the salt that makes your body hold onto water and raises blood pressure, phosphorus, a mineral that builds up when kidneys fail, weakening bones and damaging blood vessels, and potassium, an electrolyte that can cause dangerous heart rhythms if levels get too high. You don’t need to eliminate them entirely—just learn which foods pack the most punch. For example, processed meats, canned soups, and frozen meals are sodium bombs. Dairy, nuts, and whole grains are high in phosphorus. Bananas, potatoes, and oranges are potassium heavyweights. Swap them out: choose apples instead of oranges, white rice instead of brown, and fresh chicken over deli slices.
It’s not just about avoiding bad stuff—it’s about filling your plate with what helps. Lean proteins in controlled portions keep your muscles strong without overloading your kidneys. Healthy fats from olive oil or avocado support heart health, which matters because kidney disease and heart problems often go hand in hand. Drinking the right amount of fluids is tricky—too much causes swelling and shortness of breath, too little stresses your kidneys. Your doctor or dietitian will give you a daily limit based on your stage of disease. And don’t forget: many herbal supplements and over-the-counter meds can hurt your kidneys even more. Things like ginkgo, licorice root, or even some painkillers need to be checked before you take them.
People with chronic kidney disease often juggle multiple meds—blood pressure pills, diuretics, phosphate binders—and each one interacts with food. That’s why the right diet doesn’t just help your kidneys—it makes your medications work better. Lower sodium means your blood pressure meds don’t have to work as hard. Controlling phosphorus means your binders do their job without extra side effects. This isn’t a one-size-fits-all plan. What works for someone in stage 3 might not fit someone on dialysis. That’s why the posts below give you real, practical advice: how to read food labels, what swaps actually work, how to handle cravings, and how to talk to your doctor about your diet without feeling overwhelmed. You’ll find tips on managing side effects from medications, cutting down on polypharmacy risks, and making daily choices that add up to real health gains.
Renal Nutrition: Protein Targets for CKD Stages Explained
Learn the right protein targets for each stage of chronic kidney disease. Discover how much to eat, which sources are best, and how to avoid muscle loss while protecting your kidneys.
- November 13 2025
- Tony Newman
- 9 Comments
