Kidney Disease Protein Intake: What to Eat and What to Avoid
When you have kidney disease, a condition where the kidneys can’t filter waste and fluid properly. Also known as chronic kidney disease, it means your body needs careful management of what you eat—especially protein. Too much protein forces your kidneys to work harder, speeding up damage. Too little can leave you weak and prone to infection. Finding the right balance isn’t about cutting protein entirely—it’s about choosing the right amount and type for your stage of disease.
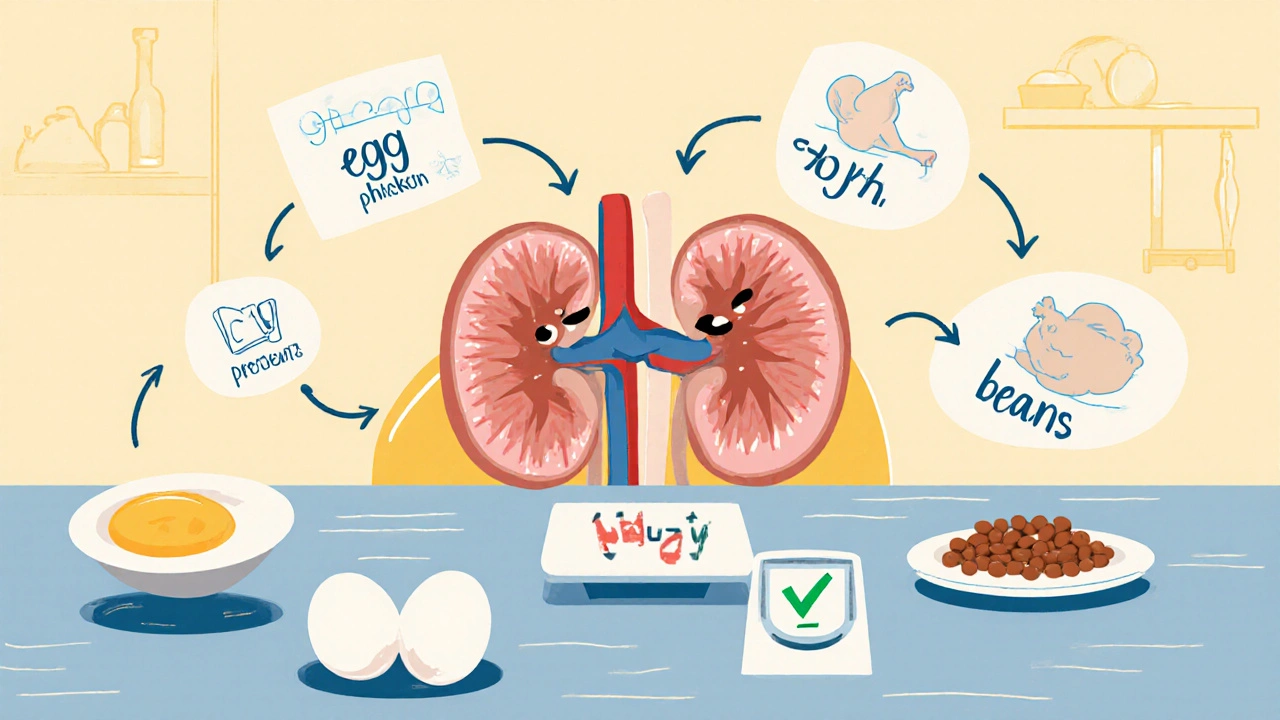
Protein intake, the amount of protein consumed daily, directly affects how much waste builds up in your blood. For early-stage kidney disease, doctors often recommend 0.6 to 0.8 grams of protein per kilogram of body weight. For someone weighing 70 kg, that’s about 42 to 56 grams a day. That’s less than most people think—roughly the size of a deck of cards in meat or two eggs plus a small serving of beans. Kidney-friendly foods, low-phosphorus, low-potassium options that reduce strain on the kidneys include egg whites, skinless chicken, fish, and plant-based proteins like tofu in moderation. Avoid processed meats, canned soups, and dairy-heavy meals—they’re packed with hidden sodium and phosphorus that your kidneys can’t handle well.
Many people with kidney disease also struggle with chronic kidney disease diet, a structured eating plan designed to slow progression and manage symptoms. It’s not just protein. It’s also controlling fluids, sodium, potassium, and phosphorus. A diet high in fruits and vegetables sounds healthy—but bananas, oranges, potatoes, and tomatoes can raise potassium to dangerous levels. Instead, swap them for apples, cabbage, cauliflower, or grapes. You don’t need to count every gram, but you do need to be aware of portion sizes and food choices. This isn’t a fad diet. It’s medical advice backed by decades of clinical practice.
Some folks think cutting protein means eating only salads. That’s a myth. You still need enough protein to keep muscles strong, fight infections, and heal wounds. The trick is using high-quality, low-waste proteins—like egg whites or lean fish—and spreading them evenly through the day. A small portion at breakfast, lunch, and dinner works better than one big steak at night. Many people see better lab results, fewer hospital visits, and more energy once they adjust their intake.
What you eat doesn’t just affect your kidneys—it affects your whole body. Poor protein management can lead to muscle loss, fatigue, and even heart problems. That’s why working with a renal dietitian is one of the most effective things you can do. They don’t just give you a list. They help you build meals you actually enjoy, fit your lifestyle, and stick with long-term.
The posts below give you real, practical ways to manage your protein intake without feeling deprived. You’ll find tips on reading labels, swapping foods, tracking portions, and understanding how medications interact with your diet. Whether you’re newly diagnosed or managing kidney disease for years, these guides help you take control—one meal at a time.
Renal Nutrition: Protein Targets for CKD Stages Explained
Learn the right protein targets for each stage of chronic kidney disease. Discover how much to eat, which sources are best, and how to avoid muscle loss while protecting your kidneys.
- November 13 2025
- Tony Newman
- 9 Comments
