Low Protein Diet for Kidneys: What Works and What to Avoid
When your kidneys aren’t working well, too much protein can make things worse. A low protein diet for kidneys, a dietary approach that limits protein intake to reduce the workload on damaged kidneys. Also known as a renal diet, it’s one of the most effective, evidence-backed ways to slow the progression of chronic kidney disease without drugs. This isn’t about starving yourself—it’s about choosing the right amount and type of protein so your body gets what it needs without overloading your kidneys.
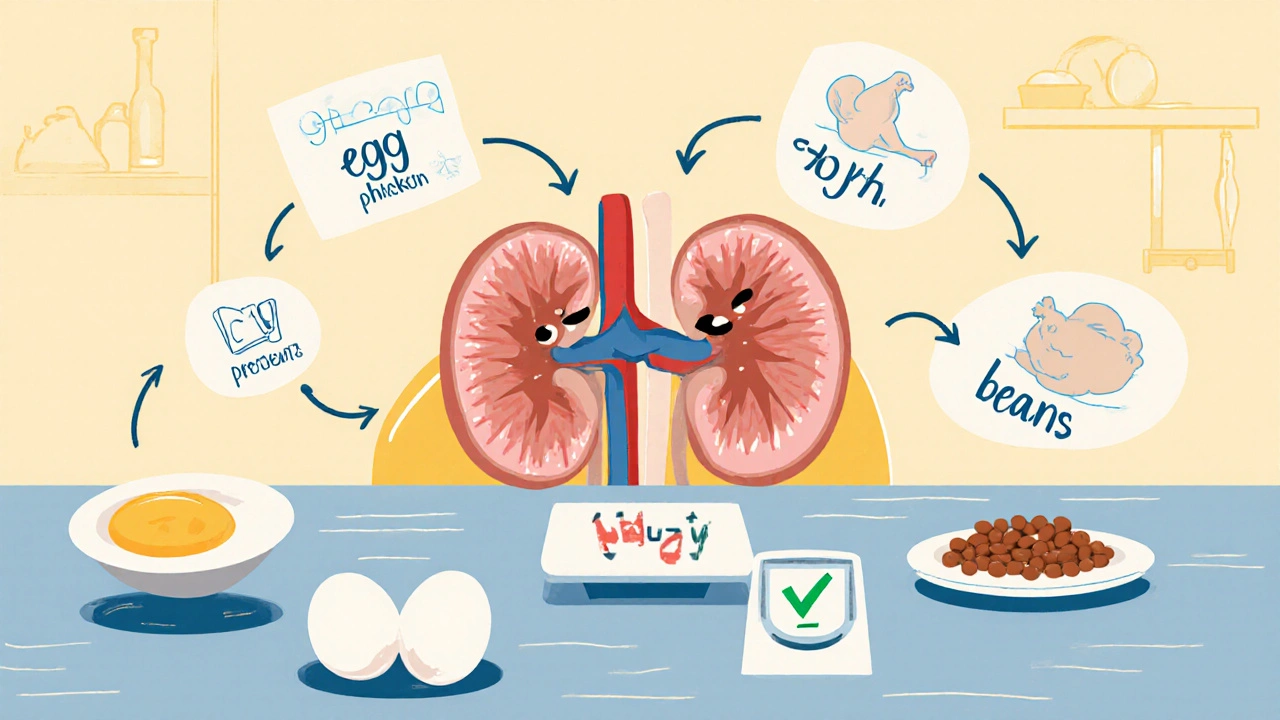
People with kidney disease often need to cut back on protein because their kidneys can’t filter waste products like urea and creatinine efficiently. When protein breaks down, it leaves behind these toxins. If your kidneys are weak, those toxins build up, making you feel tired, nauseous, or swollen. Studies show that reducing protein to about 0.6–0.8 grams per kilogram of body weight per day can help delay the need for dialysis. That’s roughly 40–50 grams a day for most adults—less than what’s in two chicken breasts. You don’t need to cut protein entirely, but you do need to be smart about where it comes from. Animal proteins like red meat, dairy, and eggs create more waste than plant proteins like beans, lentils, and tofu, so swapping some animal sources for plant ones can make a real difference.
This diet doesn’t work in isolation. It connects directly to other health habits you’re probably already managing. For example, if you’re on blood thinners or diuretics like Lasix, your fluid and electrolyte balance is already delicate. A low protein diet can help reduce fluid retention and lower blood pressure, which means you might need fewer meds—or at least fewer side effects. It also pairs well with renal diet, a structured eating plan designed to support kidney function by limiting sodium, phosphorus, and potassium along with protein. Many people don’t realize that high phosphorus from processed meats or dairy can harm bones and blood vessels even more than protein itself. And if you’re dealing with swelling or high blood pressure, the same protein restriction, a key component of kidney-friendly nutrition that reduces metabolic stress on renal filters. helps reduce fluid buildup.
There’s a lot of confusion out there. Some think cutting protein means eating only vegetables, but that’s not enough. Others think they can eat as much chicken as they want as long as they skip the salt. Neither is right. The goal is balance: enough protein to keep muscle strong, but not so much that your kidneys are drowning in waste. That’s why working with a dietitian who knows kidney health is critical. They can help you pick the right foods, adjust portions, and avoid hidden protein in things like protein bars, shakes, or even some breads.
You’ll find real-world tips here—how to stretch a small portion of meat across meals, what snacks won’t spike your numbers, how to read labels without getting overwhelmed, and how this diet fits with other health changes like walking more or managing stress. You’ll also see how this ties into broader medication safety, like avoiding supplements that might interfere with your kidneys or worsen side effects from drugs like bisoprolol or diuretics. This isn’t about perfection. It’s about making small, smart choices that add up over time—and keeping your kidneys working as long as they can.
Renal Nutrition: Protein Targets for CKD Stages Explained
Learn the right protein targets for each stage of chronic kidney disease. Discover how much to eat, which sources are best, and how to avoid muscle loss while protecting your kidneys.
- November 13 2025
- Tony Newman
- 9 Comments
