What Exactly Is Acute Kidney Injury?
Acute Kidney Injury (AKI) isn’t just a slow decline-it’s a sudden drop in how well your kidneys work, often happening over hours or days. You might not feel anything at first. In fact, about 22% of cases show no symptoms at all. That’s why it’s often caught only after a routine blood test shows your creatinine levels have spiked. Your kidneys filter waste, balance fluids, and regulate electrolytes. When they suddenly struggle, toxins build up, fluid pools in your body, and your blood chemistry goes off-kilter. This isn’t a minor glitch. It’s a medical emergency that needs fast action.
How Do You Know If You Have It?
The most obvious sign is less urine. If you’re peeing less than 400 mL in a day (oliguria) or not at all (anuria), that’s a red flag. But here’s the catch: some people keep making normal amounts of urine even when their kidneys are badly damaged-especially if there’s a blockage downstream. Other symptoms are easy to miss. Fatigue hits hard-75% of patients report it. Nausea, swelling in the legs, shortness of breath from fluid in the lungs, chest pain, or even confusion in older adults can all point to AKI. If you’ve been sick with vomiting, diarrhea, or a high fever, and now you’re feeling unusually tired or puffy, don’t wait. Get checked.
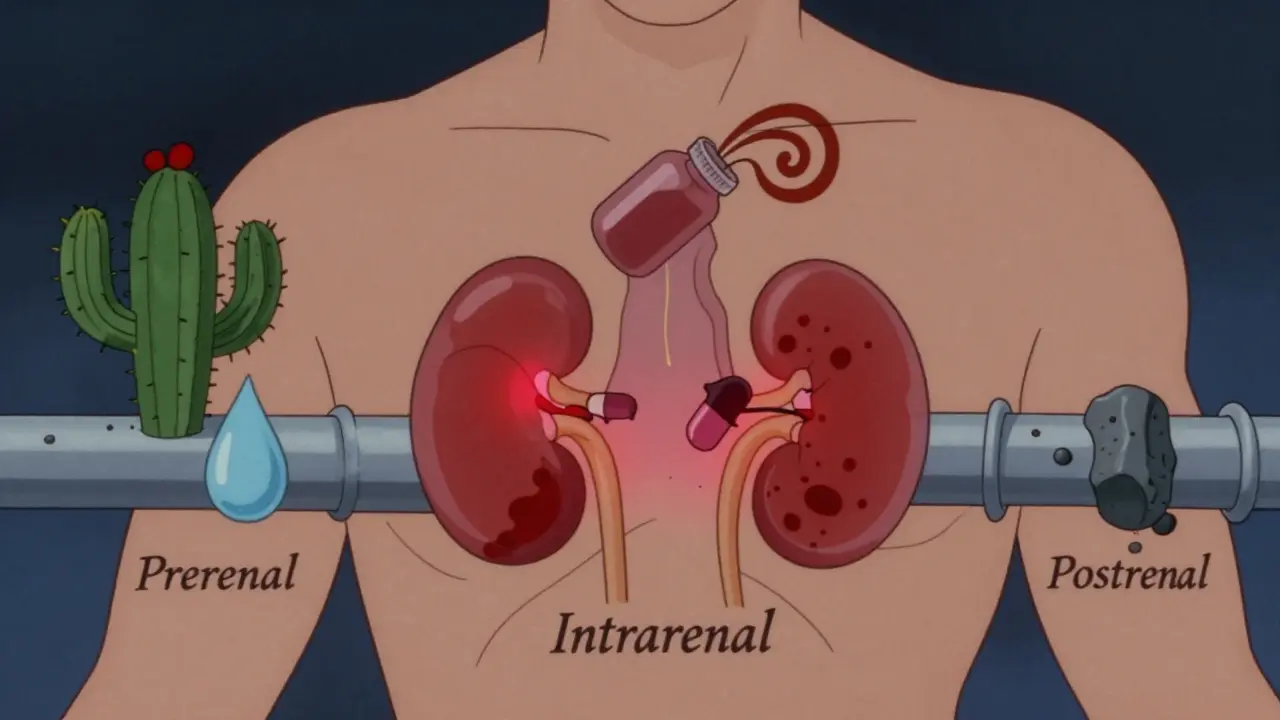
What Causes AKI? Three Main Paths
AKI doesn’t happen randomly. It follows three clear patterns, each needing a different fix.
- Prerenal (60-70% of cases): Your kidneys aren’t getting enough blood. This could be from severe dehydration after the flu, heavy bleeding, low blood pressure from infection, or heart failure. The kidneys are fine-they’re just starving for blood flow.
- Intrarenal (25-35%): The kidneys themselves are damaged. This often comes from drugs like certain antibiotics or contrast dye used in CT scans. It can also come from severe infections, autoimmune diseases like lupus, or muscle breakdown after a traumatic injury. The most common form here is acute tubular necrosis, where the kidney’s filtering units die off.
- Postrenal (5-10%): Something’s blocking the flow of urine out of your body. In men over 60, an enlarged prostate is the top culprit. In others, it’s kidney stones, tumors, or blood clots in the ureters. Even one blocked ureter can cause trouble, but two are usually needed to trigger full AKI.
How Is It Diagnosed?
Doctors don’t guess. They measure. The gold standard is the KDIGO 2012 guidelines. AKI is confirmed if your serum creatinine rises by at least 0.3 mg/dL in 48 hours, or by 50% or more in 7 days, or if you’re peeing less than 0.5 mL per kg of body weight per hour for 6 hours. Blood tests also check BUN levels and sodium balance. A urine test called fractional excretion of sodium (FeNa) helps tell if the problem is upstream (prerenal) or inside the kidney (intrarenal). Ultrasound is used in 85% of cases to rule out blockages-like stones or an enlarged prostate-before moving to more invasive tests.

What Happens If It’s Not Treated?
Left alone, AKI doesn’t just linger-it escalates. Fluid overload can flood your lungs, making breathing impossible. Potassium builds up dangerously in your blood (hyperkalemia), which can stop your heart. Acid levels rise, throwing your entire metabolism off. You might develop pericarditis-an inflammation around the heart-causing sharp chest pain. And even if you survive, the damage doesn’t always reverse. About 23% of people who recover from AKI develop chronic kidney disease within a year. Each episode raises your long-term risk of needing dialysis by over eight times.
How Is It Treated? It Depends on the Cause
There’s no one-size-fits-all fix. Treatment targets the root cause.
- Prerenal: Give fluids. Fast. A 500-1000 mL saline bolus often fixes it within a day or two. No fancy drugs needed-just restore blood flow.
- Intrarenal: Stop the poison. If a drug like an antibiotic or contrast dye caused it, stop it immediately. For autoimmune damage like glomerulonephritis, steroids or immunosuppressants are used. In rare cases like hemolytic uremic syndrome, plasmapheresis (filtering the blood) can reverse damage if done within 24 hours.
- Postrenal: Unblock it. A stent placed in the ureter to bypass a stone or enlarged prostate works in 90% of cases within hours. Catheters or surgery may be needed for other blockages.
For the worst cases-when toxins are building up, potassium is sky-high, or fluid is drowning the lungs-dialysis becomes necessary. About 5-10% of hospitalized AKI patients need intermittent hemodialysis. In the ICU, 15-20% get continuous renal replacement therapy (CRRT), which is gentler for unstable patients. Peritoneal dialysis is rare, used only when veins are too damaged for standard access.
Can You Recover Fully?
Yes-sometimes. But recovery isn’t guaranteed.
- Prerenal AKI: 70-80% recover completely if caught early, often within a week.
- Intrarenal AKI: Only 40-60% bounce back fully. Recovery takes weeks, and some damage may be permanent.
- Severe ATN with prolonged low urine output: Only 20-30% regain full function.
Age matters. If you’re over 65, your chances of full recovery drop by 35%. If your kidneys were already weak before (eGFR under 60), recovery is half as likely. Needing dialysis? Only 25% get back to normal kidney function within three months. The longer AKI lasts beyond seven days, the worse your odds.

What’s Life Like After AKI?
Recovery isn’t just about numbers on a lab report. Many survivors say they feel exhausted for months-even after their creatinine returns to normal. A 2022 survey found 68% of AKI survivors battled what they called “kidney fatigue” for 3-6 months. Anxiety about their kidneys lingered in 42%. Some needed to take time off work because they couldn’t walk more than 50 feet without gasping. One man, after 17 days on CRRT for sepsis-induced AKI, said the fear of needing lifelong dialysis was worse than the physical pain.
But recovery stories exist too. One person caught stage 1 AKI from dehydration-creatinine jumped from 0.9 to 1.8. Two liters of IV fluids in the ER, and it dropped back to 1.0 in 24 hours. Full recovery in five days. No long-term damage.
What’s New in AKI Care?
Doctors aren’t waiting for creatinine to rise anymore. New biomarkers like NGAL (neutrophil gelatinase-associated lipocalin) can predict AKI 24-48 hours before creatinine changes. Hospitals using these tests are seeing 30% better early intervention rates. In research labs, new tools like TIMP-2 and IGFBP7 can predict severity 12 hours before symptoms hit-with 85% accuracy. AI systems are being trained to scan electronic health records and flag patients at risk of AKI 12-24 hours before it happens. Early trials suggest this could cut AKI rates by 20-30%.
How to Protect Yourself
If you’re at risk-diabetic, elderly, on blood pressure meds, or recently hospitalized-stay alert. Drink water when you’re sick. Avoid NSAIDs like ibuprofen if you’re dehydrated. Tell every doctor you see about your kidney history. Ask for creatinine checks after major procedures or new medications. If you’re in the hospital, make sure staff are checking your urine output hourly. Simple steps can make all the difference.
Why This Matters
AKI adds $10,000 to $15,000 to every hospital stay. In the U.S. alone, it costs $10 billion a year. But beyond the money, it’s about lives. For every person who dies from AKI, there are two more who survive with lasting kidney damage. The window to save kidney function is narrow-often just 6 to 12 hours after the insult. Systems that catch it early-like automated alerts in hospital computers-have already lowered death rates by 12%. We know how to prevent this. We just need to act faster.
Can acute kidney injury be reversed?
Yes, in many cases-especially if caught early. Prerenal AKI, caused by dehydration or low blood pressure, often fully reverses with fluids and time. Intrarenal AKI from drug toxicity or infection can also improve, but recovery takes longer and may be incomplete. Severe cases, especially those requiring dialysis, have lower recovery rates. The key is speed: the sooner treatment starts, the better the outcome.
What are the first signs of acute kidney injury?
The earliest signs are often subtle: reduced urine output, unexplained fatigue, swelling in the legs or ankles, nausea, or confusion-especially in older adults. But many people have no symptoms at all. That’s why routine blood tests during hospital stays or after illness are critical. A sudden rise in creatinine or BUN levels is often the first objective clue.
Is acute kidney injury the same as chronic kidney disease?
No. AKI is sudden and often reversible. Chronic kidney disease (CKD) develops over months or years and is usually permanent. But AKI can lead to CKD. About 23% of AKI survivors develop stage 3 or worse CKD within a year. Each episode of AKI increases your risk of needing dialysis later by more than eight times.
Can medications cause acute kidney injury?
Yes. Common offenders include NSAIDs (ibuprofen, naproxen), certain antibiotics (like aminoglycosides), contrast dye used in CT scans, and some blood pressure drugs (especially ACE inhibitors or ARBs) when combined with dehydration. Always tell your doctor about all medications you’re taking, especially before procedures or if you’re ill.
How long does it take to recover from acute kidney injury?
Recovery time varies. Prerenal cases often resolve in 1-2 days with fluids. Intrarenal injury may take weeks to months. If you had prolonged low urine output or needed dialysis, recovery can take 3-6 months or longer-and may not be complete. Even after kidney function returns, many people feel tired for months. Follow-up care with a nephrologist is essential.
What can I do to prevent acute kidney injury?
Stay hydrated, especially when sick or after sweating. Avoid NSAIDs if you’re dehydrated or have existing kidney issues. Tell every healthcare provider about your kidney history. Get creatinine checked after major illness, surgery, or starting new meds. If you’re hospitalized, ask if your urine output is being tracked hourly. Early detection saves kidneys.