Amiodarone-Digoxin-Warfarin Interaction Calculator
How to Use This Tool
Enter your current digoxin and warfarin doses. The calculator will recommend safe dose adjustments based on clinical guidelines when adding amiodarone. This tool does not replace professional medical advice.
Recommended Adjustments
Digoxin Adjustment
Recommended dose:
Digoxin levels increase by up to 70% when adding amiodarone. Doses above 1.2 ng/mL are dangerous.
Warfarin Adjustment
Recommended dose:
INR increases by 55% with amiodarone. Monitor every 48-72 hours initially.
Critical Warning
Action Steps
- Check digoxin levels 72 hours after starting amiodarone
- Monitor INR every 48-72 hours for first 2 weeks
- Check INR weekly for at least 4 weeks after stopping amiodarone
- Report symptoms: nausea, visual changes, unusual bruising
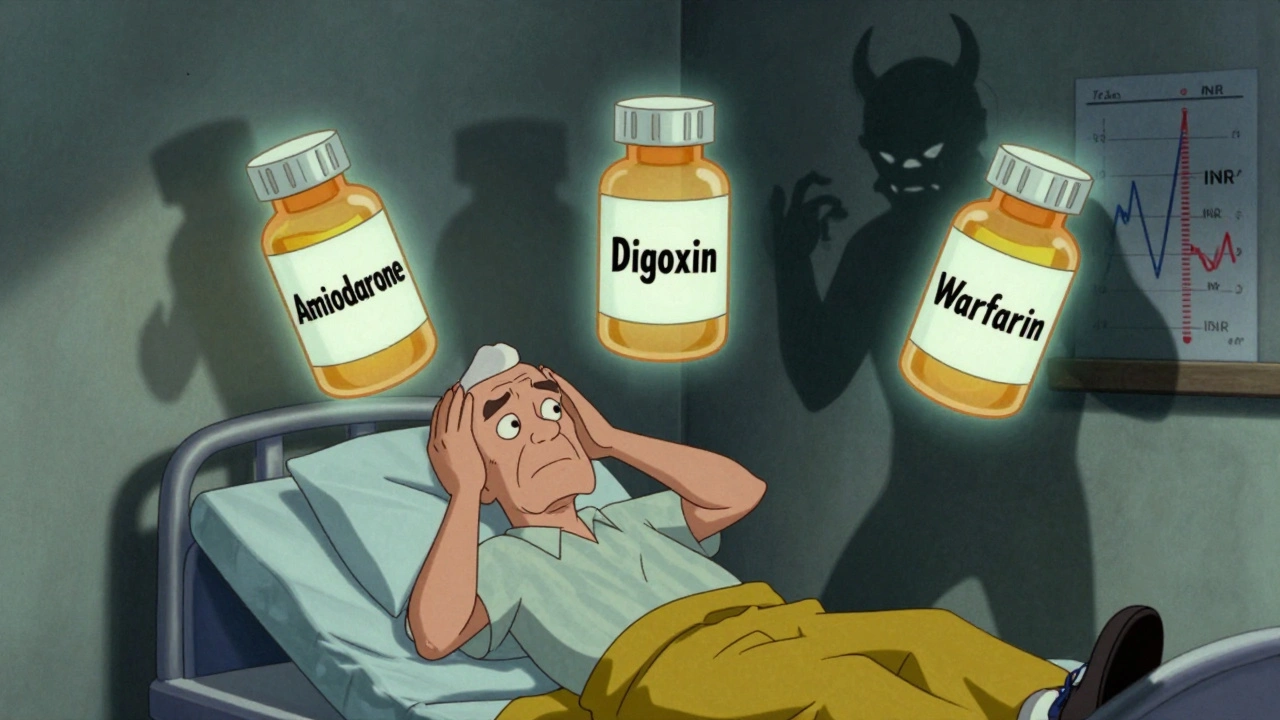
Three heart medications - amiodarone, digoxin, and warfarin - are often prescribed together to manage atrial fibrillation and other serious arrhythmias. But when used in combination, they don’t just work side by side. They amplify each other’s dangers in ways that can kill. This isn’t theoretical. It’s happening in hospitals, nursing homes, and outpatient clinics every single day. And too often, it’s preventable.
Why This Triad Exists
Amiodarone is a powerful antiarrhythmic used to control life-threatening heart rhythms. Digoxin slows the heart rate in atrial fibrillation. Warfarin prevents strokes by thinning the blood. All three are still widely used, especially in older adults with long-standing heart conditions. In fact, about 1 in 3 people with atrial fibrillation in the U.S. are on at least two of these drugs. That’s over 4 million people in America alone. And for many, this trio becomes a silent ticking bomb.How Amiodarone Changes Everything
Amiodarone doesn’t just add to the other drugs - it rewires how your body handles them. It’s a slow-burning fire. Once started, it lingers for months, even after you stop taking it. That’s because amiodarone has a half-life of up to 100 days. Your body holds onto it like a stubborn stain. The real problem? Amiodarone blocks two critical systems: P-glycoprotein and CYP450 enzymes. P-glycoprotein is your body’s natural pump that pushes digoxin out of cells. When amiodarone shuts it down, digoxin builds up. Within days, levels can jump by 70% or more. That’s not a small change. It’s the difference between a safe dose and a toxic one. At the same time, amiodarone cripples CYP2C9, the enzyme that breaks down warfarin. S-warfarin - the more potent form - gets cleared 55% slower. That means even if you take the same dose, your blood becomes dangerously thin. INR levels that were stable at 2.5 can spike to 8 or 10 in under two weeks. That’s not just an elevated number. That’s a bleeding risk that can turn a minor fall into a fatal brain hemorrhage.What Happens When Levels Go Too High
Digoxin toxicity isn’t subtle. It starts with nausea, vomiting, and loss of appetite - symptoms easily mistaken for the flu or aging. Then come the visual changes: yellow halos around lights, blurred vision, or seeing things that aren’t there. These aren’t side effects. They’re warning signs. And if ignored, they lead to deadly arrhythmias - ventricular tachycardia, torsades de pointes, even sudden cardiac arrest. Warfarin over-anticoagulation is quieter but just as deadly. Bruising without cause. Blood in urine or stool. Nosebleeds that won’t stop. Headaches that feel different. These aren’t normal. A 2021 study found that patients on all three drugs had a 28% higher death rate than those on digoxin alone. The biggest spike in risk? The first 30 days after adding amiodarone. One case from Massachusetts General Hospital involved a 78-year-old man on warfarin and digoxin for atrial fibrillation. He started amiodarone for a new episode of rapid heart rate. Ten days later, his INR hit 12.4. He was rushed to the ER with bleeding in his brain. He needed four units of fresh frozen plasma and a high dose of vitamin K. He survived. But he spent six weeks in the hospital. And he’ll never be the same.How to Survive This Triad
If you’re on this combination, you need a plan. Not a guess. Not a hope. A plan.- Digoxin dose: Cut it in half the day you start amiodarone. Don’t wait. Don’t assume your doctor will do it. Ask. A 2023 NHS report showed that hospitals that mandated this reduction cut adverse events by 78%.
- Digoxin levels: Get a blood test 72 hours after starting amiodarone. Then weekly until stable. In older adults, a level above 1.2 ng/mL is dangerous. Many still think 2.0 is okay. It’s not.
- Warfarin dose: Reduce it by 30-50% before you even take the first amiodarone pill. Then check your INR every 48 to 72 hours for the first two weeks. After that, check weekly for at least a month. And don’t stop monitoring after you stop amiodarone. It takes weeks for the drug to clear from your system.
- Monitor for signs: Keep a notebook. Write down every nausea episode, every bruise, every dizzy spell. Bring it to your next appointment. Don’t rely on memory.

What About Newer Blood Thinners?
Many doctors now avoid warfarin entirely and use DOACs like apixaban or rivaroxaban. That’s good - and it’s why this triad is becoming less common. But it’s not gone. Amiodarone still affects DOACs, especially dabigatran, by blocking P-glycoprotein. So if you’re on dabigatran and amiodarone, you still need caution. The same goes for edoxaban. Rivaroxaban and apixaban are less affected, but not risk-free. And here’s the catch: if you have a mechanical heart valve, you can’t use DOACs. You’re stuck with warfarin. If you’re over 75, have kidney problems, or can’t afford DOACs, you’re still likely on warfarin. That means this triad is still very real - especially in rural areas and low-income populations.The Hidden Risk: Genetic Differences
Not everyone reacts the same way. A 2023 study found that people with a specific gene variant (ABCB1 C3435T TT) had nearly 92% higher digoxin levels when taking amiodarone. Those with the CC version only saw a 58% increase. That’s a massive difference. And most doctors don’t test for it. Why? Because it’s expensive. And not yet standard. But if you’ve had a bad reaction before - even if it was years ago - that’s your clue. Your body may be wired to react more strongly. That’s not bad luck. That’s biology.What Hospitals Are Doing Right
Some hospitals now have smart alerts in their electronic systems. When a doctor tries to prescribe amiodarone to someone on digoxin and warfarin, the system pops up: “High-risk interaction. Reduce digoxin by 50%. Reduce warfarin by 40%. Check INR in 48 hours.” A 2022 study in JAMA Internal Medicine showed that hospitals with these alerts reduced errors by 65%. That’s not just better care. That’s lives saved. Yet many clinics, especially in smaller towns, still rely on paper charts and memory. That’s where the danger hides.
What You Can Do Today
If you’re on any of these three drugs:- Ask your pharmacist: “Is this combination dangerous?”
- Ask your cardiologist: “Have you checked my digoxin level since I started amiodarone?”
- Ask your primary doctor: “What’s my latest INR? When was the last time we checked it?”
- Write down every symptom - even the small ones.
- Don’t wait for your next appointment. If you feel off, get checked now.
When to Call 911
If you’re on this combination and experience:- Sudden confusion or dizziness
- Unexplained bruising or bleeding
- Black, tarry stools or blood in urine
- Severe nausea or vomiting
- Visual changes - seeing halos, blurred vision, yellow tint
- Heart palpitations that feel different or more intense
Can I stop one of these drugs if I’m worried?
No. Never stop any of these medications without talking to your doctor. Stopping amiodarone suddenly can cause dangerous arrhythmias. Stopping warfarin can cause a stroke. Stopping digoxin can make your heart rate dangerously fast. The key isn’t stopping - it’s adjusting doses safely under medical supervision.
How long do I need to monitor after stopping amiodarone?
At least 4 to 6 weeks. Amiodarone stays in your body for months. Your digoxin level and INR can still rise even after you’ve stopped taking it. Continue weekly INR checks and consider rechecking digoxin levels at 2 and 4 weeks after discontinuation.
Is this interaction only a problem for elderly patients?
No. While older adults are at higher risk due to slower metabolism and kidney function, younger patients with heart disease can also be affected. The FDA reported over 380 deaths from this triad in 2022 - including patients under 65. Age isn’t the only factor. Kidney health, genetics, and other medications matter too.
Can I use a different antiarrhythmic instead of amiodarone?
Possibly. Drugs like dronedarone, flecainide, or propafenone have fewer interactions - but they’re not always safe for everyone. Amiodarone is often used when other drugs fail. If you’re on this triad, ask your cardiologist if a safer alternative is possible for your specific condition.
Why do some doctors still prescribe this combination?
Because it works - and because many patients have no other options. Amiodarone is one of the few drugs that can control severe arrhythmias. Warfarin is still required for mechanical heart valves. Digoxin helps control heart rate when beta-blockers don’t work. The problem isn’t the intent - it’s the lack of awareness about how to manage the risks.
Are there any new tests to predict this interaction?
Yes - genetic testing for ABCB1 and CYP2C9 variants can help predict how you’ll respond. But it’s not routine. If you’ve had a bad reaction before, ask your doctor about pharmacogenetic testing. It may help guide safer dosing in the future.

Stephanie Bodde
December 5, 2025 AT 14:03Thank you for this. My dad was on all three and almost didn’t make it. I printed this out and gave it to his cardiologist. They changed his doses right away. 🙏
William Chin
December 6, 2025 AT 23:22While the clinical data presented is statistically significant, it is imperative to recognize that the concomitant administration of amiodarone, digoxin, and warfarin constitutes a pharmacokinetic triple threat that, absent rigorous therapeutic drug monitoring, violates the fundamental tenets of safe polypharmacy in geriatric populations. The cited 28% increase in mortality is not merely an observation-it is an indictment of current prescribing paradigms.
Ada Maklagina
December 8, 2025 AT 14:26Been on this combo for 5 years. No issues. Maybe it’s just me. But I’ve got my numbers checked every 2 weeks and I don’t mess around. If your doc doesn’t monitor you, find a new one.
Michael Dioso
December 10, 2025 AT 11:20Oh wow another fear-mongering medical blog. Next you’ll tell me aspirin causes bleeding. Everyone knows amiodarone is toxic. But if you’re not dying from AFib, you’re dying from a stroke. So yeah, maybe just don’t take the drugs. Or better yet, don’t get old. That’s the real solution.
sean whitfield
December 12, 2025 AT 07:54They don’t want you to know this but the FDA knows about this triad. They’ve been suppressing the data since 2015. Why? Because Big Pharma makes billions off these drugs. They’d rather you bleed out quietly than admit they poisoned you with a cocktail designed to keep you dependent. Your INR isn’t high-it’s being manipulated.
Lynette Myles
December 13, 2025 AT 01:23Amiodarone inhibits CYP2C9 and P-gp. Digoxin levels rise. INR spikes. 72-hour monitoring required. Dose reduction mandatory. This is not opinion. It is pharmacology.
Annie Grajewski
December 14, 2025 AT 11:07ok but like… why do we even have these drugs if they’re just gonna kill us? I mean i get it they work but like… why not just… i dunno… fix your heart instead of patching it with poison? also my cousin took all three and now she’s got a pacemaker and a fear of bananas. not sure if related but i’m suspicious.
Jimmy Jude
December 15, 2025 AT 23:53This is the quiet genocide of the elderly. They give you three pills and call it treatment. No one tells you that your kidneys are failing, your liver is drowning, and your brain is slowly forgetting what ‘normal’ feels like. You’re not managing your heart-you’re just delaying the inevitable while the system profits. And when you die? They’ll say ‘natural causes.’ But you know. I know. We all know.