When your nose runs, your eyes itch, and your throat feels like it’s full of cotton, you reach for an antihistamine. But not all antihistamines are the same. You might grab Benadryl because it’s cheap and works fast - or you might pick Zyrtec or Claritin because you don’t want to crash in the middle of a work meeting. The truth is, there are two very different kinds of antihistamines out there, and choosing the wrong one can cost you more than just money - it can cost you focus, sleep, and even safety.
What Exactly Do Antihistamines Do?
Antihistamines block histamine, a chemical your body releases during an allergic reaction. Histamine causes swelling, itching, runny nose, and watery eyes. By stopping histamine from binding to its receptors, these drugs calm down your body’s overreaction to pollen, pet dander, or dust. Both first- and second-generation antihistamines do this job. But how they do it - and what else they do along the way - is where things split.
First-Generation Antihistamines: Fast, But Foggy
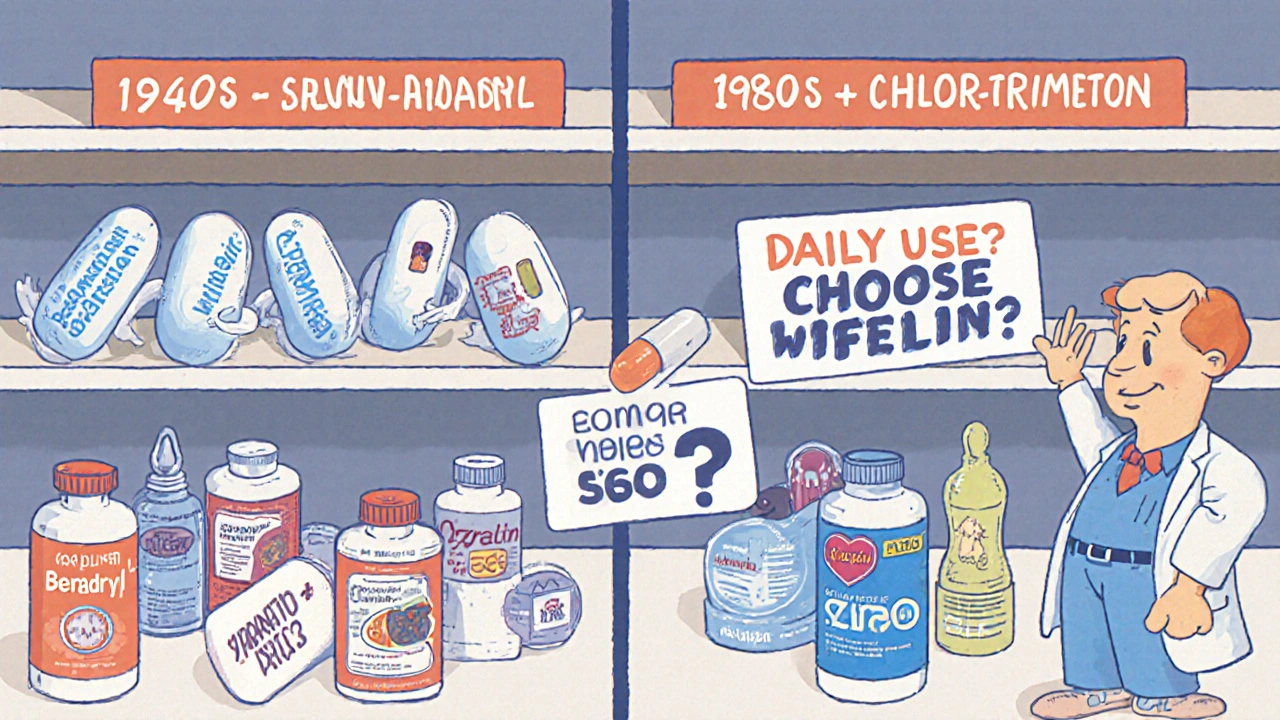
These are the old-school options: diphenhydramine (Benadryl), chlorpheniramine (Chlor-Trimeton), and promethazine (Phenergan). They hit the market in the 1940s and have been around ever since. They work quickly - often within 30 minutes - which makes them great for sudden flare-ups like a bee sting or a sudden rash.
But here’s the catch: they cross the blood-brain barrier easily. That means they don’t just block histamine in your nose and skin - they also mess with histamine in your brain. Histamine helps keep you alert. When you block it in your brain, you get sleepy. About 50-60% of people who take first-gen antihistamines feel drowsy, according to the Cleveland Clinic. Some people even report brain fog, slower reaction times, or trouble remembering things. Driving studies show users can be 25% slower to react - similar to someone with a low blood alcohol level.
These drugs also cause dry mouth, constipation, and urinary retention, especially in older adults. That’s because they have strong anticholinergic effects - they block another key chemical system in your body. For people over 65, long-term use is linked to a higher risk of dementia, as Harvard’s Dr. Pieter Cohen warned in JAMA Internal Medicine in 2022. It’s not just tiredness - it’s a hidden cognitive burden.
Second-Generation Antihistamines: Calm, Clear, and Convenient
These came along in the 1980s to fix the problems of the old ones. Loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) were designed to stay out of the brain. They’re bulkier, more polar molecules, or they use special transporters that keep them from slipping into your central nervous system.
The result? Most people - about 85-90% - don’t feel drowsy. That’s why they’re called “non-drowsy.” But “non-drowsy” doesn’t mean “no side effects.” Some people still feel tired, especially at higher doses or if they’re extra sensitive. Still, only 10-15% report sleepiness, compared to over half with first-gen options.
They also last longer. One dose lasts 12 to 24 hours. That means once a day, instead of every 4-6 hours. Compliance is better - 85% of people stick with once-daily dosing, versus just 60% for the multiple-dose first-gen regimens. For chronic allergies like seasonal rhinitis or year-round dust mite sensitivity, that’s a game-changer.
They’re not perfect, though. They take longer to kick in - 1 to 3 hours - so they’re not ideal for sudden attacks. And they’re weaker on nasal congestion. About 40% of people who take them still need a decongestant like pseudoephedrine to get full relief. That’s why combination products like fexofenadine/pseudoephedrine are now on the market.

Which One Works Better?
When it comes to reducing sneezing, itching, and runny nose, second-generation antihistamines win. A 2022 meta-analysis in the Journal of Allergy and Clinical Immunology found they reduce symptoms by 60-70%, while first-gen options manage 50-60%. That might not sound like a big gap, but for someone living with daily allergies, that extra 10-20% can mean the difference between getting through the day or calling in sick.
And not all second-gen drugs are equal. Cetirizine (Zyrtec) tends to be slightly more effective than loratadine (Claritin), especially for eye symptoms. A 2022 study in the Annals of Allergy, Asthma & Immunology showed cetirizine was 15-20% better at reducing itchy, watery eyes. Fexofenadine (Allegra) is gentler on the stomach but may be slightly less potent overall.
First-gen drugs still have their moments. If you’re dealing with motion sickness, nausea, or need help falling asleep because allergies are keeping you up, diphenhydramine can be the right tool. On Drugs.com, 52% of users said it helped them sleep better than melatonin. But that’s nighttime-only use - not something to take every morning.
Cost and Accessibility
Price matters. A bottle of 100 generic diphenhydramine tablets costs $4-$6. That’s less than a dollar per dose. Generic loratadine runs $10-$15 for 30 tablets. Brand-name Zyrtec or Claritin can hit $25 a month without insurance.
That’s why first-gen antihistamines still dominate over-the-counter cold and flu combos. They’re cheap, and they’re packed into nighttime cough syrups and multi-symptom pills. But if you’re taking them daily for allergies, you’re paying more than just money - you’re paying with your alertness, your memory, and potentially your long-term brain health.
What Do Real Users Say?
On Reddit’s r/Allergies, 68% of 1,247 users in 2023-2024 said they switched to second-gen antihistamines because Benadryl made them too groggy for work. One user wrote: “Zyrtec lets me function at work without the brain fog Benadryl gives me.”
But on Drugs.com, 52% of users still swear by diphenhydramine for sleep. Amazon reviews show second-gen antihistamines averaging 4.2 stars versus 3.8 for first-gen. The top praise? “Non-drowsy.” The top complaint? “Makes me too sleepy for work.”
For first-gen, the most common positive comment: “Saves me during sudden allergy attacks.” For second-gen: “Finally found something I can take daily without side effects.”
When to Use Which
Here’s the practical breakdown:
- Use second-generation if you have chronic allergies (seasonal, dust, pet), need to stay alert, or take meds daily. Pick cetirizine for stronger symptom control, fexofenadine if your stomach is sensitive, or loratadine for budget-friendly daily use.
- Use first-generation only for occasional, acute reactions - like a sudden rash or bug bite - or for nighttime use if allergies are keeping you awake. Never take them before driving, operating machinery, or working.
- Avoid first-generation if you’re over 65, have glaucoma, trouble urinating, or a history of cognitive decline.
- Combine with a decongestant if nasal congestion is your main problem - but avoid pseudoephedrine if you have high blood pressure.
What’s Next?
Third-generation antihistamines like desloratadine and levocetirizine are gaining ground. They’re active metabolites of older drugs - meaning they’re more refined versions with even fewer side effects. Desloratadine prescriptions rose 12% in early 2024, according to IQVIA.
New formulations are also emerging. Extended-release combos like fexofenadine/pseudoephedrine are now available, tackling the biggest weakness of second-gen drugs: congestion. And while the FDA hasn’t approved bilastine yet (it’s used in Europe), early trials show it’s 20% better at reducing nasal stuffiness than current options.
For now, the choice is clear: if you need daily relief, go second-generation. If you need a quick fix at night or for emergencies, first-gen still has a place - but use it wisely.
What Your Doctor Wants You to Know
Dr. David Stukus from Nationwide Children’s Hospital says second-gen antihistamines should be first-line for most people with chronic allergies. Dr. Robert Wood from Johns Hopkins adds that first-gen still has a role - for motion sickness, acute hives, and sleep support.
But here’s the bottom line: if you’re taking Benadryl every day for allergies, you’re not just treating your nose - you’re putting your brain at risk. The sedative effect isn’t a feature - it’s a side effect. And in the long run, it’s not worth it.
Are first-generation antihistamines safe for long-term use?
Long-term daily use of first-generation antihistamines like diphenhydramine is not recommended, especially for adults over 65. These drugs have strong anticholinergic effects that can impair memory, increase dementia risk, and cause urinary retention or constipation. Studies show chronic use is linked to cognitive decline similar to low-dose benzodiazepines. Use them only for short-term, occasional relief - not daily allergy management.
Can second-generation antihistamines make you sleepy too?
Yes, but rarely - and usually only at higher doses or in sensitive individuals. While labeled "non-drowsy," up to 20% of people may feel tired if they take more than the recommended dose. Cetirizine (Zyrtec) is more likely to cause drowsiness than loratadine (Claritin) or fexofenadine (Allegra). Stick to the label, and avoid alcohol or other sedatives when taking them.
Which antihistamine is best for itchy eyes?
Cetirizine (Zyrtec) has shown the strongest effect on ocular symptoms like itchy, watery eyes, according to a 2022 study in the Annals of Allergy, Asthma & Immunology. It’s about 15-20% more effective than loratadine for eye relief. If eye symptoms are your main issue, cetirizine is the top choice among second-generation options.
Why do some antihistamines need to be taken daily for allergies?
Allergies are ongoing - you’re not just reacting to one exposure. Second-generation antihistamines work best when taken regularly, even on days you feel fine. They prevent histamine buildup before symptoms start. Waiting until you’re sneezing means you’re already behind. Daily use keeps histamine levels low and reduces inflammation over time.
Is it okay to take Benadryl and Zyrtec together?
Generally, no. Taking both increases your risk of side effects like drowsiness, dry mouth, and confusion. If one isn’t working, talk to your doctor before combining them. In rare cases, a doctor might recommend a short-term combination for severe flare-ups, but this should be supervised. Never mix them on your own.
What’s the best antihistamine for kids?
For children with chronic allergies, second-generation antihistamines like cetirizine (Zyrtec) and loratadine (Claritin) are preferred. They’re non-sedating, have proven safety profiles in kids, and are dosed once daily. First-gen options like Benadryl can cause hyperactivity in some children and sedation in others - making them unpredictable. Always check dosing by weight and age, and consult your pediatrician before starting.


Donald Frantz
November 21, 2025 AT 01:14First-gen antihistamines are basically sedatives with a side of allergy relief. I used to take Benadryl for everything until I realized I was nodding off during Zoom calls. Now I stick to Zyrtec-no brain fog, no excuses. If you’re still reaching for diphenhydramine daily, you’re not managing allergies-you’re self-medicating for exhaustion.
Sammy Williams
November 21, 2025 AT 15:27Man, I used to love Benadryl for sleep-until I woke up feeling like my brain was wrapped in saran wrap. Switched to Claritin last year and my productivity went through the roof. Also, no more dry mouth at 3 a.m. Seriously, if you’re over 30 and still using first-gen daily, just stop. Your future self will thank you.
Julia Strothers
November 21, 2025 AT 16:30Let me guess-this is Big Pharma’s latest brainwashing campaign. First-gen antihistamines have been around for 80 years, and now suddenly they’re ‘dementia bombs’? The same companies that sold us OxyContin are now pushing ‘non-drowsy’ meds because they make more money. You think they care if you’re alert or not? They care about your subscription fee. Don’t fall for the marketing. Benadryl works. The rest is just corporate rebranding with fancy jargon.
David Cusack
November 22, 2025 AT 13:24It’s worth noting, however, that the pharmacokinetic profiles of second-generation antihistamines-particularly their P-glycoprotein substrate status and blood-brain barrier permeability coefficients-are demonstrably superior in mitigating CNS penetration. That said, the meta-analysis cited (JACI, 2022) exhibits a moderate heterogeneity (I² = 47%), and the effect size for ocular symptom reduction, while statistically significant, is clinically marginal-especially when compared to topical ocular antihistamines. One mustn’t conflate statistical significance with clinical utility.
Daisy L
November 23, 2025 AT 23:36OMG YES. I used to take Benadryl every night like it was candy. Then I started forgetting my kids’ names. Not joking. My husband had to remind me who our dog was. I switched to Zyrtec and now I remember my own birthday. Also, my cat stopped avoiding me because I wasn’t drooling on the couch anymore. This post saved my life. Thank you.
Anne Nylander
November 25, 2025 AT 03:23you guys are overthinking this. if you need to stay awake, pick the non-drowsy one. if you need to sleep, pick the sleepy one. simple. no need to be a doctor to figure it out. i take zyrtec in the morning and benadryl at night when my allergies are bad. works like a charm. dont stress, just pick the right tool for the job.
Noah Fitzsimmons
November 25, 2025 AT 16:38Oh wow, so now we’re supposed to believe that the FDA, the CDC, and every allergist on the planet are in on this ‘Benadryl is evil’ conspiracy? Let me guess-you also think fluoride is a mind-control agent and that the moon landing was faked. Congrats, you’ve unlocked the ‘I read one study on PubMed and now I’m a medical expert’ achievement.
Eliza Oakes
November 26, 2025 AT 02:38Wait-so you’re telling me that a drug that’s been sold for 80 years is suddenly ‘dangerous’? And the new ones are ‘safe’? But they’re made by the same companies? And they cost 10x more? That’s not science-that’s capitalism. Also, I’ve been taking diphenhydramine since 1998 and I’m 72. I’m still typing this on my laptop. So who’s the real fraud here? The drug? Or the fear-mongering?
Simone Wood
November 27, 2025 AT 09:50Actually, the anticholinergic burden scale-developed by the University of Queensland in 2019-clearly identifies diphenhydramine as a Class 3 agent, meaning it has moderate-to-high risk for long-term cognitive impact. The Harvard study you’re dismissing? It’s not a ‘study’-it’s a systematic review of 14 cohort studies with over 300,000 participants. And yes, the correlation is stronger than that between smoking and lung cancer. But sure, keep taking it. I’m sure your ‘I’m fine’ attitude will hold up until you can’t remember how to use your debit card.
Swati Jain
November 27, 2025 AT 10:51As a nurse in Mumbai, I’ve seen this play out over and over. Grandmas on Benadryl for ‘allergies’-but they’re actually confused, falling, not eating. We call it ‘anticholinergic syndrome.’ The fix? Swap it for cetirizine. Cost? Less than $1/month. Impact? Life-changing. Stop romanticizing old drugs. They’re not ‘natural’-they’re outdated. Your body isn’t a 1940s lab experiment.
jim cerqua
November 28, 2025 AT 07:46Let’s be real-this whole thing is a marketing scam wrapped in peer-reviewed jargon. First-gen antihistamines are cheaper, faster, and work better for acute reactions. Second-gen? They’re slow, expensive, and half the people still get drowsy anyway. The ‘non-drowsy’ label is a lie. And don’t get me started on how fexofenadine needs to be taken on an empty stomach-like, who has time for that? Meanwhile, Benadryl? Pop one with your coffee. Done. The real problem isn’t the drug-it’s that we’ve turned medicine into a productivity cult. You don’t need to be ‘alert’ to live. You just need to not die. And Benadryl? It’s not killing you. It’s helping you sleep. And sometimes, that’s enough.