Antiplatelet Drug Selection Tool
This tool helps you understand which P2Y12 inhibitor drug might be most appropriate for your situation based on your medical history and lifestyle. It's designed to help you have informed discussions with your doctor. Always consult your healthcare provider before making any changes to your medication.
Your Recommendation
Your doctor will determine the best medication based on your complete medical history and individual risk factors. This tool provides general guidance based on your input.
- Loading...
When you’ve had a heart attack or a stent placed, your doctor gives you a blood thinner-not to thin your blood like water, but to stop your platelets from clumping together and forming dangerous clots. Three drugs do this job better than most: clopidogrel, prasugrel, and ticagrelor. They’re all P2Y12 inhibitors, meaning they block a specific receptor on platelets to keep them from sticking. But they’re not the same. One might save your life, while another could leave you gasping for air or bleeding internally. Choosing the right one isn’t just about science-it’s about your body, your life, and your risks.
How These Drugs Work (And Why It Matters)
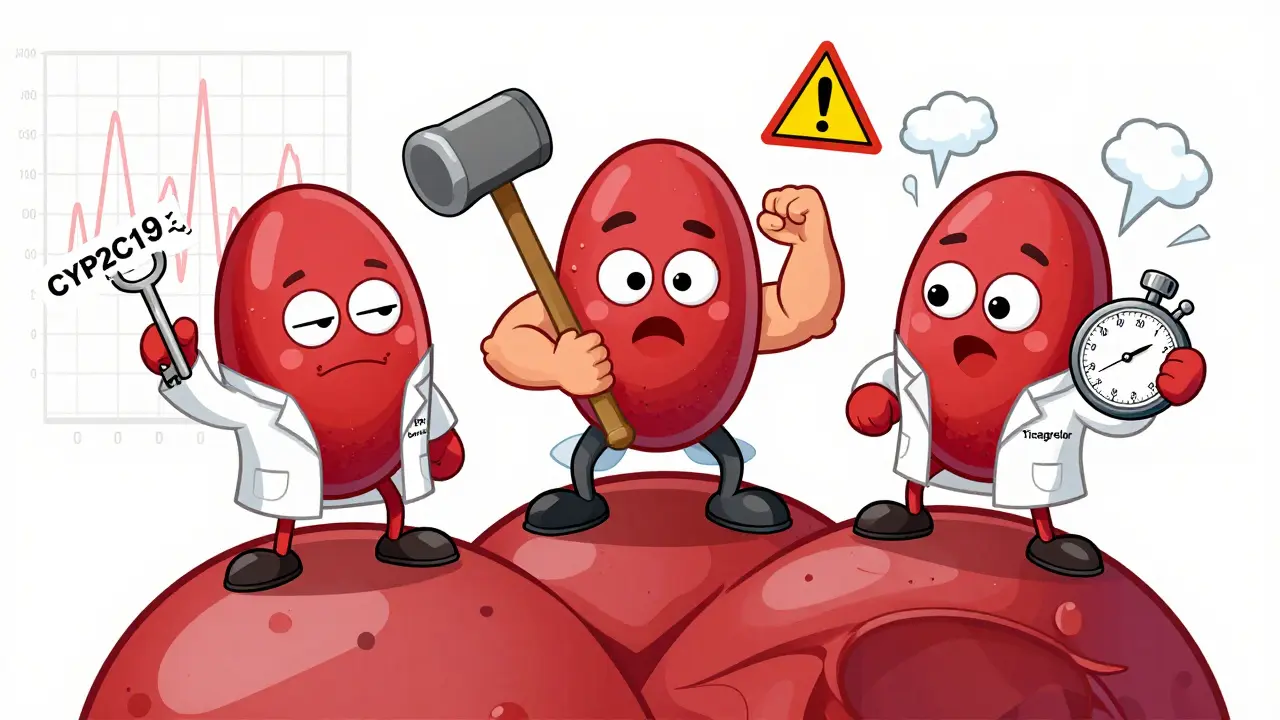
All three drugs stop platelets from clumping, but they do it in different ways. Clopidogrel and prasugrel are prodrugs. That means your liver has to convert them into their active form before they work. Ticagrelor? It’s already active when you swallow it. This difference changes everything-how fast they kick in, how strong they are, and how predictable they are. Clopidogrel is the oldest. It’s been around since 1997. But about 30% of people don’t respond well to it. Why? Genetics. If you have a CYP2C19 gene variant (common in Asians and some Caucasians), your body can’t turn clopidogrel into its active form. You’re taking a pill that does almost nothing. That’s why some patients still have heart attacks even while on clopidogrel. Prasugrel is stronger. It’s converted more efficiently by the liver, so it blocks platelets faster and more completely. Ticagrelor doesn’t need conversion at all. It works in 30 minutes and reverses quickly when you stop taking it. That’s good news if you need emergency surgery. But it also means you have to take it twice a day, every day-no skipping.The Biggest Risk: Bleeding
All three drugs increase your risk of bleeding. That’s not a side effect-it’s the trade-off. You can’t stop clots without sometimes letting blood leak where it shouldn’t. In the TRITON-TIMI 38 trial, prasugrel cut heart attacks and stent clots better than clopidogrel-but it also caused more major bleeding. Specifically, 2.4% of prasugrel users had serious bleeding compared to 1.8% on clopidogrel. Fatal bleeding? Four times higher. That’s why prasugrel comes with a black box warning from the FDA: don’t use it if you’ve had a stroke or are over 75. Ticagrelor, in the PLATO trial, reduced heart-related deaths compared to clopidogrel. But it also increased non-surgical major bleeding-2.6% vs. 2.3%. That might sound small, but in a population of 10,000 patients, that’s 30 extra people bleeding badly. Gastrointestinal bleeding happens in about 1% of users. Intracranial bleeding? Rare-0.1% to 0.3%-but devastating when it happens. And here’s the catch: prasugrel’s bleeding risk shoots up in people under 60 kg (about 132 lbs) or over 75. One cardiologist told me he saw an 80-year-old woman’s hemoglobin drop from 12 to 8 g/dL in two weeks on prasugrel. She didn’t need a transfusion, but she was hospitalized. That’s why many doctors avoid prasugrel in frail elderly patients-even if they’re high risk for clots.Ticagrelor’s Hidden Side Effect: Can’t Breathe
If you’ve never heard of ticagrelor causing shortness of breath, you’re not alone. But it’s real. In the PLATO trial, 14% to 16% of people on ticagrelor reported dyspnea-feeling like they couldn’t catch their breath. That’s compared to 8% to 10% on placebo. The risk? 1.7 times higher. It’s not anxiety. It’s not heart failure. It’s a direct effect of the drug. Patients describe it as “drowning in air,” “like a weight on my chest,” or “I could breathe, but it felt wrong.” It usually starts within days. Most don’t get worse. Many get used to it. But 15% to 20% of patients stop taking it because of it. And here’s what doctors don’t always tell you: if you have asthma or COPD, this side effect can be worse. One patient in Melbourne told me she’d been on ticagrelor for six months after a stent. “I thought I was getting sicker,” she said. “Turned out, it was the drug. My doctor switched me to clopidogrel, and within three days, I could walk to the mailbox without stopping.” Ticagrelor also causes brief pauses in your heartbeat-ventricular pauses. In the PLATO trial, 3.1% had them vs. 2.0% on clopidogrel. Usually harmless. But if you have a pacemaker or a history of slow heart rhythms, your doctor needs to know.
Cost, Convenience, and Compliance
Clopidogrel costs about $10 a month as a generic. Ticagrelor and prasugrel? Around $300 to $400. That’s why clopidogrel is still used in 60% of cases, even though it’s less effective for some. Ticagrelor requires two pills a day. Miss a dose? Your protection drops fast. Prasugrel is once daily. Clopidogrel? Once daily too. But if you’re a CYP2C19 poor metabolizer, once daily doesn’t matter-it’s useless. Adherence matters. A 2018 study found people on ticagrelor were 21% more likely to stop taking it because of side effects than those on clopidogrel. That’s not just about discomfort-it’s about survival. If you stop, your risk of clotting skyrockets in the first month.When to Choose Which Drug
Here’s what cardiologists actually do in real life:- Prasugrel is the go-to for young, high-risk patients-under 75, no history of stroke, over 60 kg-who’ve had a heart attack and are getting a stent. It’s the strongest clot blocker. But if you’re frail, elderly, or weigh less than 132 lbs? Avoid it.
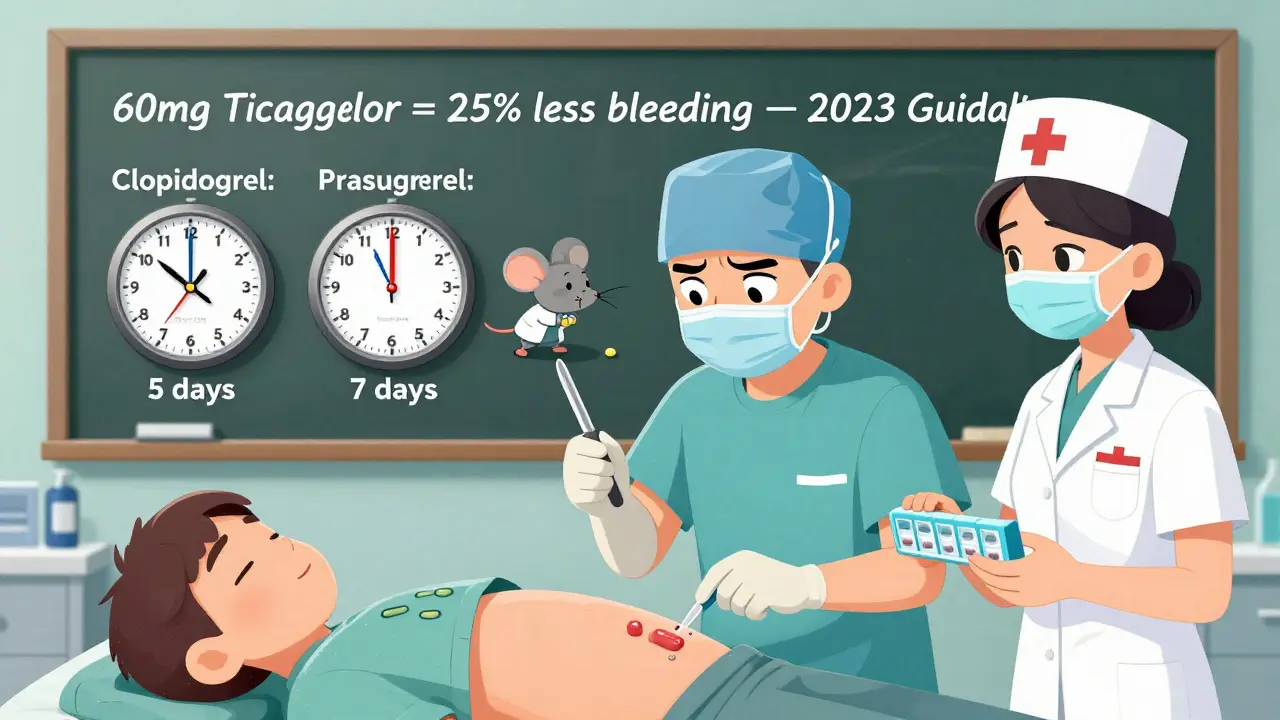
- Ticagrelor is preferred for almost all ACS patients, including those treated with meds alone (not PCI). It reduces death rates. But if you have lung disease, or you’re worried about breathlessness, your doctor might skip it. The new 60 mg twice-daily dose (approved in 2023) is a game-changer for long-term use-it cuts bleeding by 25%.
- Clopidogrel is still used for cost reasons, or if you can’t tolerate the others. But if you’re Asian, or you’ve had a stent and still had a clot? Ask about genetic testing. It’s $200 to $300. Not covered everywhere. But if you’re a poor metabolizer, switching to ticagrelor could save your life.
What Happens Before Surgery?
If you need surgery-dental, knee replacement, even a colonoscopy-you need to stop these drugs. But not at the same time.- Clopidogrel: stop 5 days before
- Prasugrel: stop 7 days before
- Ticagrelor: stop 3 days before
What’s New in 2026?
The 2023 ACC/AHA guidelines now recommend tailoring how long you stay on dual therapy (aspirin + P2Y12 inhibitor). For high-risk patients: 6 to 12 months. Then switch to low-dose ticagrelor (60 mg twice daily) or just aspirin. This cuts bleeding without raising clot risk. New drugs are coming. Selatogrel, a subcutaneous P2Y12 inhibitor, is in phase 3 trials. It’s fast-acting, reversible, and might be used in emergencies-like if you’re having a heart attack and can’t swallow a pill.What Should You Do?
If you’re on one of these drugs:- Know your dose. Don’t guess.
- Know your risk. Are you over 75? Under 60 kg? Have you had a stroke? If yes, ask if prasugrel is right for you.
- If you’re short of breath on ticagrelor, don’t ignore it. Tell your doctor. It might be the drug. And it might be fixable.
- If you’re on clopidogrel and had a clot anyway, ask about genetic testing.
- Never stop without talking to your cardiologist-even if you feel fine.
These aren’t just pills. They’re tools. And like any tool, they work best when you know how to use them-and when to avoid them.
Can I switch from clopidogrel to ticagrelor if I’m not responding?
Yes, but only under medical supervision. If you’re a CYP2C19 poor metabolizer, clopidogrel may not be working. Studies show switching to ticagrelor reduces the risk of heart attack or death in these patients. Your doctor can order a genetic test to confirm, but even without one, if you’ve had a clot while on clopidogrel, switching is often recommended.
Is ticagrelor safe if I have asthma?
It’s not ideal. About 1 in 7 people on ticagrelor get shortness of breath-even without asthma. If you have asthma or COPD, your risk is higher. Some doctors still prescribe it if the benefit outweighs the risk, but they’ll monitor you closely. Others avoid it entirely and use clopidogrel or prasugrel instead. Always tell your doctor about your lung history.
Why is prasugrel not recommended for people over 75?
Because bleeding risk jumps significantly. In the TRITON-TIMI 38 trial, patients over 75 on prasugrel had a 2.7% rate of major bleeding compared to 1.8% on clopidogrel. Fatal bleeding was nearly triple. The FDA black box warning specifically says not to use prasugrel in patients over 75 unless the benefit clearly outweighs the risk-which is rare. For older patients, ticagrelor or clopidogrel are safer choices.
Can I take these drugs with alcohol?
Moderate alcohol (one drink a day) is generally okay, but heavy drinking increases bleeding risk. Alcohol thins the blood a little on its own, and these drugs do too. Together, they can push you into dangerous territory. If you drink regularly, tell your doctor. You might need more frequent blood tests or a different drug.
What if I miss a dose of ticagrelor?
If you miss one dose, take it as soon as you remember. If it’s close to your next dose, skip it. Don’t double up. Missing one dose isn’t a disaster, but missing several increases your clot risk sharply. Ticagrelor’s effect fades quickly-within 24 hours. That’s why adherence is critical. Set phone reminders. Use a pill organizer. This isn’t a drug you can afford to forget.
Do I need blood tests while on these drugs?
Routine blood tests aren’t required, but your doctor might check your hemoglobin or platelet count if you’re bleeding or feeling weak. Platelet function tests exist, but they’re not standard because they’re expensive and don’t reliably predict outcomes. The best test? Pay attention to your body. Unexplained bruising, dark stools, dizziness, or shortness of breath? Call your doctor.
Is there a cheaper alternative to ticagrelor or prasugrel?
Clopidogrel is the main cheaper option. But it’s not always as effective. If cost is a barrier, ask your doctor about generic clopidogrel. Some pharmacies offer it for under $5 a month. If you’re a good candidate, it’s safe and effective. But if you’ve had a clot on clopidogrel, switching to a more potent drug-even if it costs more-could be lifesaving.

Bobby Collins
January 2, 2026 AT 04:05Ann Romine
January 2, 2026 AT 05:40Austin Mac-Anabraba
January 3, 2026 AT 02:28Phoebe McKenzie
January 4, 2026 AT 05:56gerard najera
January 5, 2026 AT 16:42Stephen Gikuma
January 7, 2026 AT 15:11Layla Anna
January 8, 2026 AT 20:36Olukayode Oguntulu
January 10, 2026 AT 20:24jaspreet sandhu
January 11, 2026 AT 15:11LIZETH DE PACHECO
January 12, 2026 AT 12:18Kristen Russell
January 14, 2026 AT 00:43Bryan Anderson
January 14, 2026 AT 05:26Matthew Hekmatniaz
January 16, 2026 AT 01:53