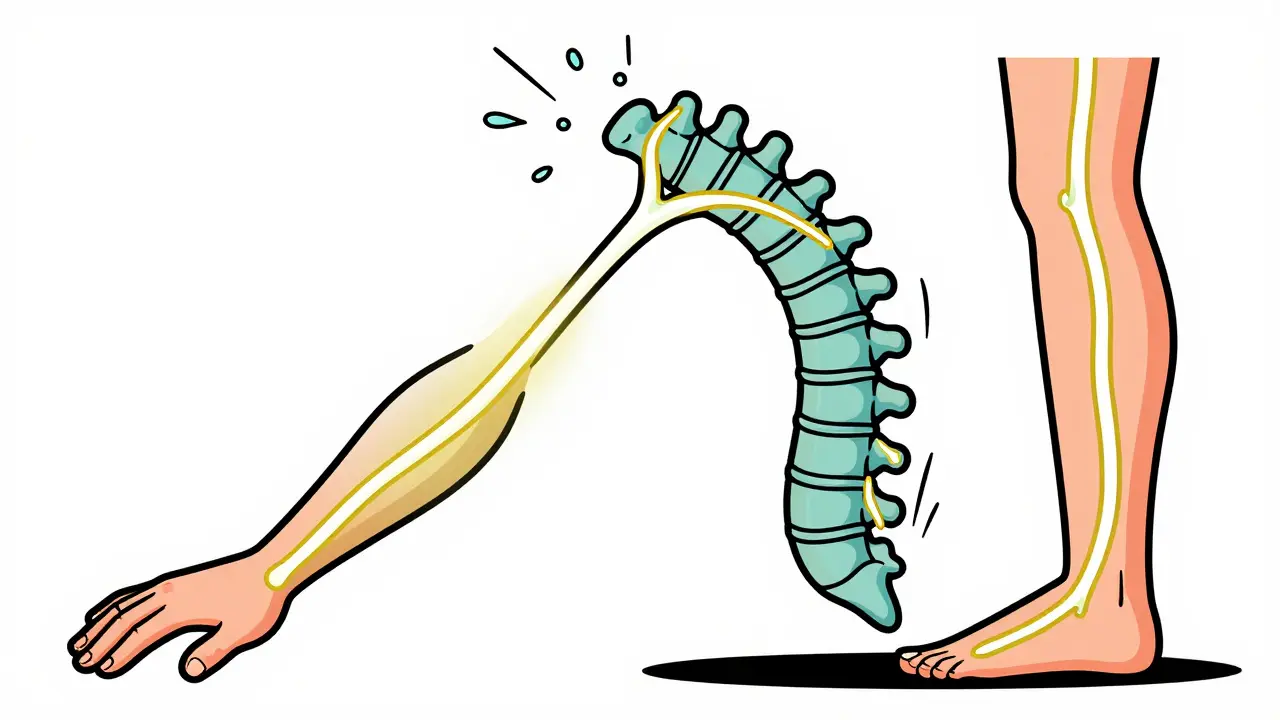
When your neck or lower back pain shoots down your arm or leg like an electric shock, it’s not just a muscle cramp. It’s radiculopathy - a pinched or irritated nerve root in your spine. This isn’t rare. About 1 in 5 adults will deal with it at some point, especially between ages 45 and 64. And while the pain can feel terrifying, the good news? Most people get better without surgery - if they know what to do.
What Exactly Is Radiculopathy?
Radiculopathy happens when a nerve root - the bundle of nerves that exit your spine - gets squeezed or inflamed. It’s not a disease. It’s a symptom. And it shows up in two main places: your neck (cervical) or your lower back (lumbar). Together, these two types make up 95% of all cases. In your neck, the problem usually starts with a bulging disc or bone spur pressing on a nerve. You might feel pain in your shoulder, tingling in your fingers, or weakness when gripping things. C7 is the most common culprit - that’s the nerve that runs down to your middle finger. If your middle finger goes numb, it’s often a sign. Down in your lower back, it’s often called sciatica. The L5 or S1 nerve gets compressed, and pain races down the back of your leg, sometimes all the way to your toes. You might drop your foot when walking, or feel like your calf is on fire. These aren’t random symptoms. They follow exact nerve paths - dermatomes - and doctors use them like maps to find the problem.Why Does It Happen? Age and Lifestyle Matter
If you’re under 50, a herniated disc is the usual suspect. One wrong lift, a car accident, or even a bad cough can pop a disc out of place and pinch the nerve. But after 50, it’s mostly wear and tear. Arthritis in the spine, narrowing of the nerve tunnels (foraminal stenosis), and thickened ligaments slowly squeeze the nerves over time. Lumbar radiculopathy is strongly tied to jobs that involve heavy lifting - construction, nursing, warehouse work. The risk jumps 3.2 times higher for people who lift regularly. Cervical radiculopathy? More linked to sudden trauma - whiplash, falls, or even sleeping in a bad position for too long. And here’s something surprising: men are slightly more likely to get lumbar radiculopathy (53% vs 47%), but cervical cases are almost evenly split. Why? Probably because men are more likely to do physically demanding jobs - but neck issues don’t care about your job title.How Do You Know It’s Radiculopathy - Not Just Back Pain?
Not every back or neck ache is radiculopathy. Here’s how to tell:- Radicular pain: It travels. Neck pain that zaps into your thumb? That’s not a stiff muscle. Lower back pain that runs down your leg to your foot? That’s nerve-related.
- Numbness or tingling: In specific spots - like your index finger (C6), middle finger (C7), or outer foot (L5).
- Weakness: Struggling to lift your arm, grip a bottle, or lift your foot when walking.
- Reflex changes: Your doctor might check your knee or ankle reflexes. A dull reflex can mean a compressed nerve.
Conservative Treatment Works - Here’s How
Eighty-five percent of people get better in 12 weeks with just conservative care. Surgery is the exception, not the rule. Phase 1: Reduce the Fire (Weeks 1-2) Start with rest - but not bed rest. Keep moving gently. Avoid heavy lifting, twisting, or long drives. Over-the-counter NSAIDs like ibuprofen (400mg three times a day) help reduce swelling around the nerve. Heat or ice? Try both. Heat relaxes tight muscles. Ice calms inflammation. Most people find ice works better in the first 48 hours. Phase 2: Physical Therapy (Weeks 2-8) This is where real progress happens. A good physical therapist won’t just give you exercises - they’ll tailor them to your nerve root. For cervical radiculopathy:- Chin tucks: Sit tall, gently pull your chin straight back. Hold 5 seconds. Do 10 reps, 3x/day. This repositions the neck and takes pressure off the nerves.
- Scapular retractions: Squeeze your shoulder blades together. Hold 3 seconds. Repeat 15 times. Strengthens the upper back, which supports the neck.
- Cervical traction: Some therapists use gentle traction (5-10 lbs of pull) for 15-20 minutes. It opens up space around the nerve. Studies show it helps 70% of patients.
- McKenzie extension exercises: Lie on your stomach, prop yourself up on your elbows. Hold for 30 seconds. Progress to full push-ups if pain allows. This moves disc material away from the nerve.
- Core stabilization: Bird-dogs, dead bugs, and planks train your deep abdominal muscles to support your spine.
- Hamstring stretches: Tight hamstrings pull on the lower spine. Stretch daily - hold each for 30 seconds.
What About Injections?
Epidural steroid injections are common - but controversial. The Cochrane Database says they give only short-term relief (2-6 weeks) with no long-term benefit. But in real life? 58% of pain specialists say they help. Why the gap? It’s about timing and patient selection. If you’ve had pain for less than 6 weeks and the pain is sharp and shooting, injections can calm the inflammation fast. If you’ve had it for 6 months and it’s dull and constant? Probably not worth it. Also, they’re not a cure. They buy you time to do physical therapy.When Surgery Might Be Needed
Surgery isn’t failure. It’s the next step when things don’t improve - or get worse. You need to see a surgeon right away if you have:- Loss of bladder or bowel control
- Severe leg weakness - you can’t lift your foot
- Progressive numbness in both legs or genitals
What Doesn’t Work (And What Could Make It Worse)
Too many people try quick fixes - and make things worse.- Returning to heavy lifting too soon: 28% of people who go back to lifting before they’re ready have a relapse.
- Doing random YouTube exercises: A Reddit user shared how crunches made their sciatica worse. Core work needs to be targeted. Wrong movements can push the nerve further.
- Ignoring posture: Slouching at your desk or sleeping on a flat pillow increases pressure on your spine. A cervical pillow that supports your neck’s natural curve helps.
- Waiting too long to start therapy: The longer you wait, the more your body learns to protect the area - which turns into chronic pain.

Real People, Real Results
A 52-year-old warehouse worker in Melbourne had L5 radiculopathy after years of lifting boxes. He tried painkillers for 3 months. Nothing changed. Then he started McKenzie exercises and core work. After 10 weeks, he could lift again - without pain. He now does 15 minutes of exercises every morning. A 48-year-old teacher had C6 radiculopathy from years of looking down at screens. She started chin tucks and scapular retractions. Within 6 weeks, her thumb numbness was gone. She now uses a monitor stand and takes 5-minute posture breaks every hour. The common thread? Consistency. Not intensity. Not expensive gadgets. Just daily movement.Long-Term Outlook
The prognosis is good. Eighty-two percent of people return to their normal activities within a year. Only 8% develop long-term chronic pain. The key? Getting moving early, staying consistent with rehab, and avoiding the traps that lead to relapse. New tech is helping too. In early 2023, the FDA approved AI software that reads MRIs with 96.7% accuracy - catching nerve compression earlier than ever. And ongoing research into targeted steroid nanoparticles and PRP injections may offer better options soon. But the most powerful tool? Still your body. Move well. Move often. And don’t wait for the pain to be gone before you start healing.Can radiculopathy go away on its own?
Yes, in most cases. About 85% of people recover fully within 12 weeks without surgery. The body naturally reduces inflammation around the nerve, and gentle movement helps the disc or bone shift slightly to relieve pressure. But waiting too long without any rehab can lead to muscle weakness and longer recovery.
Is walking good for lumbar radiculopathy?
Absolutely. Walking is one of the best low-impact activities. It increases blood flow to the spine, reduces stiffness, and gently stretches the nerves. Start with 10-15 minutes a day on flat ground. Avoid hills or uneven surfaces at first. If pain increases during or after walking, slow down - don’t stop.
Can a pillow help with cervical radiculopathy?
Yes, the right pillow makes a big difference. A pillow that supports the natural curve of your neck - not too high, not too flat - keeps your spine aligned while you sleep. Memory foam or contour pillows work best. Avoid sleeping on your stomach - it twists the neck and squeezes nerves.
Should I get an MRI right away?
Not always. If your symptoms are classic - like pain shooting down your arm or leg with numbness or weakness - and you’re otherwise healthy, doctors often recommend 4-6 weeks of conservative care first. MRIs are expensive and can show changes that aren’t causing symptoms. Only get one if pain doesn’t improve, gets worse, or if you have red flags like loss of bladder control.
What’s the biggest mistake people make with radiculopathy?
Waiting too long to start movement. Many think they need to rest until the pain is gone. But nerves heal with motion. The longer you avoid movement, the more your muscles weaken and your body learns to protect the area - which turns acute pain into chronic pain. Start gentle movement as soon as you can, even if it’s just walking or chin tucks.
Can stress make radiculopathy worse?
Yes. Stress increases muscle tension, especially in the neck and lower back. It also raises inflammation in the body, which can irritate nerves further. People under high stress often report more pain and slower recovery. Adding breathing exercises, short walks, or even 5 minutes of mindfulness each day can help reduce the body’s pain response.
Next Steps: What to Do Today
If you’re dealing with nerve pain right now:- Stop heavy lifting, twisting, or long periods of sitting.
- Take ibuprofen (400mg) up to three times a day for 3-5 days if you can.
- Start chin tucks (for neck) or McKenzie extensions (for back) - 10 reps, 2x/day.
- Use a supportive pillow at night.
- Book a physical therapy appointment within the next week.