Colchicine-Macrolide Interaction Checker
Check Your Colchicine Interaction Risk
This tool helps you determine if your antibiotic is safe to take with colchicine based on the article's medical information.
Colchicine is a simple, cheap drug. It’s been used for centuries to treat gout. Today, it’s also prescribed for heart conditions, pericarditis, and other inflammatory issues. But here’s the problem: if you take it with certain antibiotics-like clarithromycin or erythromycin-you could end up in the hospital. Or worse.
Why This Interaction Is So Dangerous
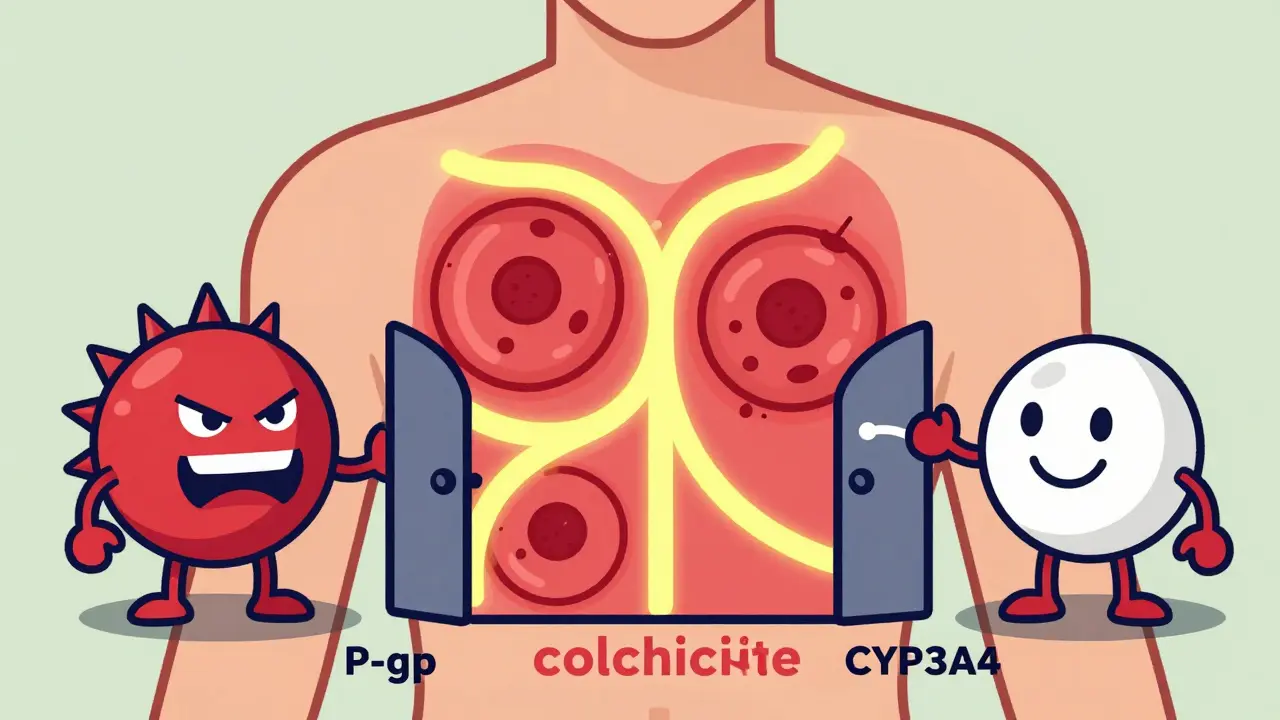
Colchicine doesn’t just float around in your blood. It gets pulled into your cells, then pushed back out by a transporter called P-glycoprotein (P-gp). At the same time, your liver uses an enzyme called CYP3A4 to break it down. Both systems work together to keep colchicine levels safe.Macrolide antibiotics like clarithromycin and erythromycin don’t just kill bacteria. They also block both P-gp and CYP3A4. When that happens, colchicine can’t get cleared. It builds up. And because the margin between a helpful dose and a toxic one is razor-thin, even a small increase can cause serious harm.
Studies show that when clarithromycin is taken with colchicine, colchicine levels can jump by up to four times. At concentrations above 3.3 ng/mL, especially in people with kidney problems, toxicity kicks in. That’s not theoretical. The FDA has a black box warning on colchicine for this exact reason.
Not All Macrolides Are the Same
It’s easy to assume all antibiotics in the same class behave the same. They don’t.- Clarithromycin: Strong inhibitor of both CYP3A4 and P-gp. Highest risk. Responsible for 63% of reported colchicine toxicity cases in FDA data.
- Erythromycin: Moderate CYP3A4 inhibitor, weaker on P-gp. Still dangerous, but less so than clarithromycin.
- Azithromycin: Minimal effect on either system. Safe to use with colchicine.
That last point matters. If you’re on colchicine and need an antibiotic, azithromycin isn’t just an option-it’s the best option. A 2022 study of over 12,000 patients found that switching from clarithromycin to azithromycin cut the risk of toxicity by 92%.
What Toxicity Actually Looks Like
Colchicine toxicity isn’t just nausea or diarrhea. Those are mild signs. Severe cases involve:- Severe muscle pain and weakness (rhabdomyolysis)
- Low white blood cell count (neutropenia)
- Bone marrow failure (pancytopenia)
- Kidney and liver failure
- Multi-organ failure and death
A 2019 case series in the Journal of Clinical Pharmacy and Therapeutics documented 12 patients who developed these symptoms after taking standard doses of colchicine with clarithromycin. Three died. Most were older adults with kidney issues-exactly the group most vulnerable.
Emergency doctors see this more often than you’d think. A 2023 survey of 245 physicians found that 82% of ER staff had treated at least one case. Rheumatologists? Only 54%. Why? Because they’re focused on gout. They don’t always think about the antibiotics their patients are taking for pneumonia or sinus infections.

Why Doctors Miss This
This isn’t just about ignorance. It’s about systems failing.Many electronic health records still don’t flag this interaction clearly. Some only warn if the patient is on a very strong inhibitor like ritonavir-but not clarithromycin. Others don’t warn at all. A 2021 study showed that 43% of internal medicine residents couldn’t identify high-risk combinations on a test.
Patients don’t always tell their doctors about over-the-counter supplements. St. John’s wort, grapefruit juice, even some herbal remedies can also inhibit CYP3A4. And if a patient is taking colchicine for heart disease, they might be on five or six other drugs. The risk multiplies.
What Should You Do?
If you’re on colchicine, here’s what you need to know:- Never take clarithromycin or erythromycin. Period.
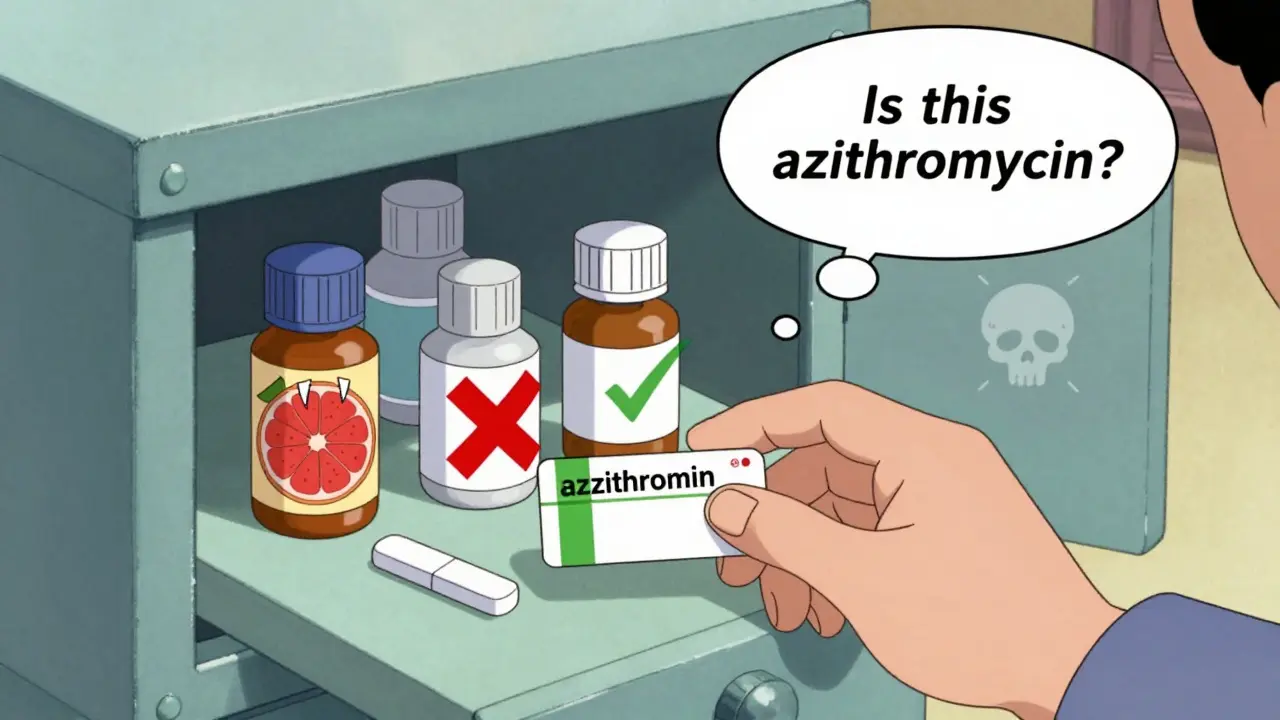
- Ask for azithromycin if you need an antibiotic. It’s just as effective for most infections and doesn’t interfere.
- Check all your meds-including supplements. Grapefruit juice, diltiazem, verapamil, amiodarone, and even some antifungals can cause the same interaction.
- If you’re on a moderate inhibitor (like fluconazole or verapamil), your colchicine dose should be cut in half.
- Know the warning signs: Unexplained muscle pain, weakness, fever, nausea, or unusual bruising/bleeding. Call your doctor immediately.
What’s Being Done to Fix This?
The problem is getting worse, not better. Since 2010, colchicine use has grown by 217% because it’s now approved for heart attack recovery and pericarditis. Meanwhile, millions of macrolide prescriptions are written every year in the U.S. alone. That’s over 1.2 million potential dangerous combinations annually.Some progress is being made. Epic’s electronic health record system updated its alerts in 2023 and reduced inappropriate prescribing by 63% in a multi-hospital trial. Hospitals are starting to train staff better. But it’s still not universal.
Research is also moving toward solutions. Takeda, the maker of colchicine, is testing a new version called COL-098 that doesn’t interact with P-gp. Early trials show it’s 92% safer with clarithromycin. That could change everything.
Another promising path? Genetic testing. A 2023 study found that two specific gene variants-CYP3A5*3/*3 and ABCB1 3435C>T-predicted 78% of colchicine toxicity cases. If you have these variants, your body clears colchicine poorly. That’s something your doctor could test for, especially if you’ve had side effects before.
Why This Matters Beyond the Prescription
Colchicine costs about $4,200 a year. The alternative for heart inflammation? Canakinumab, which costs $198,000. That’s why doctors keep prescribing colchicine-even with the risks.But here’s the truth: colchicine isn’t dangerous because it’s a bad drug. It’s dangerous because we treat it like it’s harmless. It’s not. It’s a narrow-window drug. One mistake, one missed interaction, and it can kill.
The real solution isn’t just better alerts or new versions of the drug. It’s awareness. Patients need to know. Doctors need to listen. Pharmacies need to double-check.
Because if you’re taking colchicine and your doctor says, “I’m giving you this antibiotic for your chest infection,” don’t assume it’s safe. Ask: Is this azithromycin? If not, ask why.
Can I take colchicine with azithromycin?
Yes. Azithromycin does not significantly inhibit CYP3A4 or P-gp, so it’s considered safe to take with colchicine. It’s the preferred antibiotic choice if you’re on colchicine and need treatment for an infection.
What happens if I accidentally take clarithromycin with colchicine?
Stop both medications immediately and contact your doctor or go to the emergency room. Symptoms of toxicity can develop within hours or days. Early intervention can prevent life-threatening complications like rhabdomyolysis or bone marrow failure.
Is there a blood test to check colchicine levels?
Yes, but it’s not widely available. Only about 37% of U.S. hospitals can test colchicine levels routinely. Even if the test is available, it’s usually only used in severe cases or research settings-not for routine monitoring.
Can grapefruit juice interact with colchicine?
Yes. Grapefruit juice strongly inhibits CYP3A4 in the gut, which can increase colchicine levels. Avoid it completely if you’re taking colchicine, even in small amounts.
Why isn’t this interaction more widely known?
Because colchicine is old, cheap, and not heavily marketed. Many doctors assume it’s harmless. But the data shows otherwise. The FDA issued a black box warning in 2010, and multiple studies since then confirm the risk. Awareness is improving, but it’s still lagging behind the danger.
What are safer alternatives to colchicine for gout or heart inflammation?
For gout, NSAIDs like naproxen or corticosteroids are common alternatives. For heart inflammation, canakinumab is approved but extremely expensive. Colchicine remains the most cost-effective option, so the focus is on managing its risks-not replacing it.
Final Takeaway
Colchicine isn’t going away. It’s too useful, too cheap, too effective. But it’s not a benign drug. It’s a precision tool-and like any precision tool, it needs careful handling.If you’re taking it, treat it like you would a blood thinner or chemotherapy drug. Double-check every new prescription. Ask questions. Don’t let convenience override safety.
Because sometimes, the most dangerous thing in your medicine cabinet isn’t the expensive new drug. It’s the old, cheap one you think you know.

Napoleon Huere
January 26, 2026 AT 15:51Colchicine is one of those drugs that should come with a warning label in neon lights and a bagpipe solo. We treat it like aspirin because it's cheap and old, but it's basically pharmaceutical Jenga-pull one wrong block and the whole tower collapses. Why are we still relying on a 200-year-old molecule without better safeguards? We have AI, blockchain, self-driving cars-but we can't get EHRs to flag a life-threatening interaction? That's not negligence. That's cultural laziness.
Shweta Deshpande
January 26, 2026 AT 19:05Oh my goodness, this post made me so relieved I checked my meds last week! I've been on colchicine for pericarditis and my doctor just prescribed azithromycin for a sinus infection-I didn’t even know there was a risk! Thank you for explaining it so clearly. I printed this out and gave it to my pharmacist too. We need more posts like this-real, practical, life-saving info without the jargon overload. Seriously, someone should turn this into a flyer for every pharmacy counter!
Robin Van Emous
January 27, 2026 AT 11:12I'm glad this is getting attention. I've seen this happen twice in my clinic. One patient, 72, diabetic, CKD stage 3, took clarithromycin for bronchitis and ended up in the ICU with rhabdo. He didn't know he was on colchicine-he thought it was just for his 'gout flare.' His daughter found the bottle in the cabinet. We didn't even know he was taking it. It's not the drug's fault. It's the system. We're not connecting dots. We're just prescribing.