When you’re handed a prescription, do you feel like you’re making a choice-or just accepting an order? For too many people, medication decisions still feel like something done to them, not with them. But the truth is, you have a right to control what goes into your body. That’s not just a nice idea-it’s a legal and ethical standard backed by decades of medical ethics, real-world data, and patient experiences.
Why Your Voice Matters in Medication Decisions
Medication autonomy isn’t about being difficult or rejecting doctors. It’s about recognizing that drugs aren’t just chemical solutions-they’re lifestyle changes. A pill might lower your blood pressure, but if it makes you dizzy every afternoon, you can’t drive, and you’re missing work, that’s not a win. That’s a trade-off. And only you know what trade-offs you’re willing to make. The idea that patients should have control over their medications started gaining real weight after the Nuremberg Trials in the 1940s. It wasn’t just about consent-it was about dignity. By the 1970s, U.S. courts confirmed that doctors must give you all the material information before you agree to a treatment. Today, that means knowing not just what a drug does, but what it might cost, how often you’ll need to take it, what side effects are common, and what other options exist. And it’s not just theory. In 2023, 87% of U.S. healthcare institutions claimed to use shared decision-making for medication choices. But here’s the catch: only 42% of clinics in rural or underserved areas actually do it consistently. That gap isn’t just about resources-it’s about mindset. Too often, doctors assume they know what’s best. But patients who feel heard are more likely to stick with their meds.What Real Autonomy Looks Like
Autonomy doesn’t mean you get to pick any drug you want. It means you get to make an informed decision among the options that are medically appropriate. Here’s what that looks like in practice:- You’re told the success rate of each option-for example, SSRIs help about half of people with depression, but 25-30% of those users experience sexual side effects.
- You hear about cost differences: a brand-name biologic might cost $6,000 a month, while a biosimilar costs $4,000-with similar results.
- You’re shown non-drug alternatives: therapy, diet changes, exercise, or digital tools that can help manage your condition.
- You’re asked: What matters most to you? Energy? Sleep? Avoiding needles? Not gaining weight?
Where the System Still Fails
You might think this is standard practice. It’s not. Only 45% of primary care doctors regularly use shared decision-making for medications. Compare that to surgery, where 68% do. Why? Because meds feel like they’re “easier” to manage. But that’s a dangerous assumption. Cost is a huge barrier. In 2023, 32% of Medicare Part D users changed or skipped doses because they couldn’t afford their meds. That’s not noncompliance-it’s survival. And yet, many doctors never ask about cost. They assume insurance covers it. Or worse, they assume you’ll just pay whatever’s needed. Then there’s direct-to-consumer ads. They influence 28% of patient requests for specific drugs. Sometimes that’s good-you’re informed. Other times, it’s misleading. You might ask for a drug because you saw a slick commercial, but your doctor knows it’s not right for you. Autonomy means you can ask-and your doctor should listen, explain why it might not fit, and offer better alternatives. And let’s talk about culture. A 2023 survey found that Black and Hispanic patients were significantly less likely to feel involved in medication decisions than white patients. Why? Language barriers, distrust in the system, or doctors who don’t take time to explain. Autonomy isn’t just about information-it’s about respect.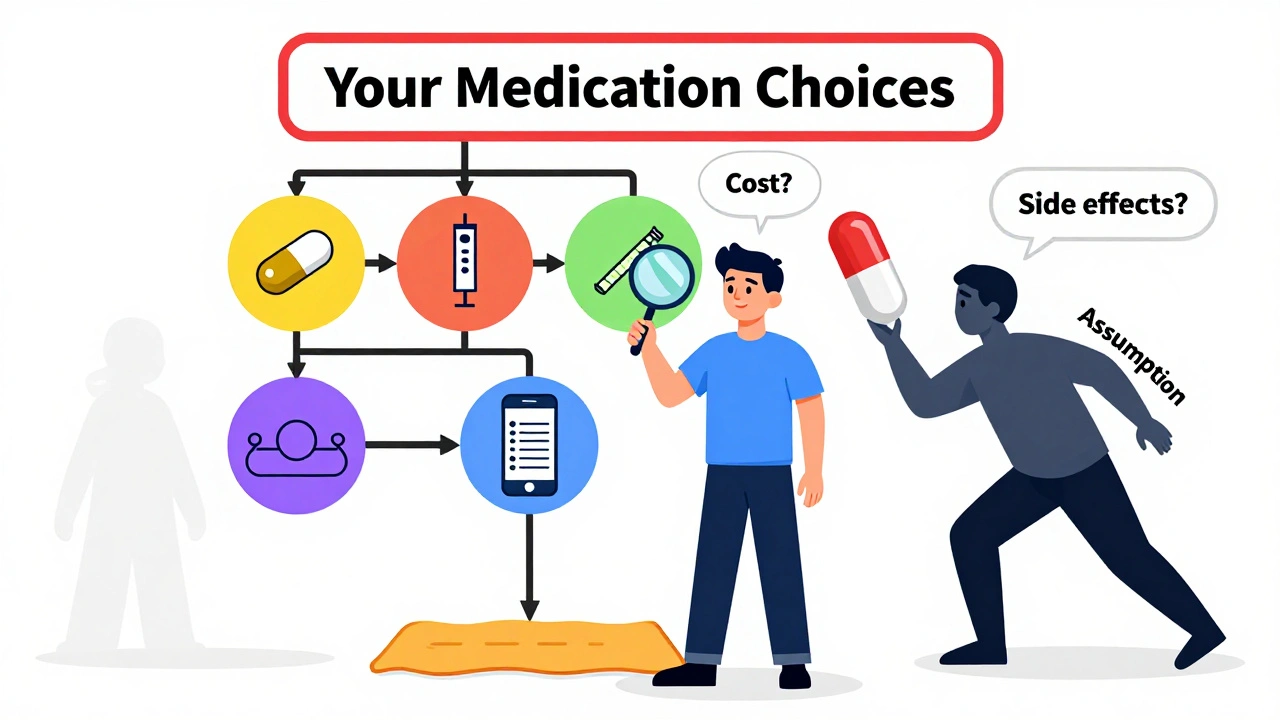
Real Stories: When Autonomy Made a Difference
One cancer patient on Reddit refused opioids because of her religious beliefs. She didn’t want to numb her pain-she wanted to stay present. Her doctor didn’t push. They worked together on a non-opioid plan that required more frequent dosing but respected her values. She stayed comfortable. She stayed in control. Another patient, managing diabetes, was prescribed Ozempic but felt sick just thinking about the nausea. She asked for alternatives. Her doctor said, “It’s the best option.” She switched providers. The new doctor offered three other options, including a once-weekly injectable that didn’t cause nausea. She’s been on it for six months. Her A1C is down. She feels like she chose her treatment-not the other way around. These aren’t outliers. They’re what autonomy looks like when it works.What You Can Do Right Now
You don’t need to be an expert to take charge of your medication choices. Here’s how to start:- Ask: “What are my options?” Not just the one you’re being given. Ask for alternatives, including cheaper ones or non-drug approaches.
- Ask: “What’s the evidence?” Not “Is this good?” but “How well does it work for people like me?”
- Ask: “What’s the cost?” Out-of-pocket. Monthly. Yearly. If you can’t afford it, say so. There are often patient assistance programs.
- Ask: “How will this affect my daily life?” Will I be tired? Will I need to take it with food? Will I have to change my schedule?
- Ask: “Can I try something else if this doesn’t work?” Make sure there’s a plan B.

What’s Changing-and What’s Coming
The system is slowly catching up. In 2024, the FDA started requiring drugmakers to collect patient preference data during development. That means future meds might be designed around what patients actually care about-not just what’s easiest to test in labs. Pharmacogenomic testing is dropping in price-from $1,200 in 2020 to $249 today. Soon, your genes might tell your doctor which drug will work best for you, with fewer side effects. That’s personalized medicine, and it’s coming fast. But here’s the problem: 37% of adults over 65 say they struggle to use digital tools for medication decisions. If tech becomes the main way we support autonomy, we risk leaving behind the very people who need it most.Autonomy Isn’t Perfect-But It’s Necessary
Some experts warn that too much autonomy can lead to bad choices. A patient might refuse antibiotics because of a viral TikTok video. That’s dangerous. But the answer isn’t to take away choice-it’s to improve the conversation. Better education. Better tools. More time. The goal isn’t for you to become a doctor. It’s for your doctor to become a partner. Someone who gives you the facts, listens to your fears, respects your values, and helps you choose-not decide-for you. Medication isn’t just about chemistry. It’s about control. About dignity. About living your life on your terms. And that’s not a privilege. It’s a right.Can I refuse a medication even if my doctor recommends it?
Yes. If you have decision-making capacity-meaning you understand the risks, benefits, and alternatives-you have the legal and ethical right to refuse any medication, even if your doctor believes it’s the best option. This right is protected under informed consent laws established since the 1970s. Your doctor should explain why they recommend it, but they cannot force or pressure you into taking it.
What if my doctor won’t discuss other options?
If your doctor dismisses your questions or refuses to talk about alternatives, it’s a red flag. You’re not being difficult-you’re exercising your right to informed choice. Try asking again, using phrases like, “I’d like to understand all my options before deciding.” If that doesn’t work, consider seeking a second opinion or switching providers. Many clinics now use shared decision-making tools, and you deserve care that respects your input.
How do I know if I’m making an informed choice?
You’re making an informed choice if you understand: (1) what the medication does, (2) how likely it is to help, (3) what side effects you might face, (4) how much it costs, (5) what alternatives exist-including non-drug options-and (6) what happens if you don’t take it. If you can answer those questions without guessing, you’re on solid ground. Ask for written materials or use trusted sources like the Mayo Clinic’s decision aids to fill in gaps.
Does autonomy mean I can choose any drug I want?
No. Autonomy means choosing from medically appropriate options-not picking any drug off the shelf. Your doctor will help narrow the choices based on your health, history, and risks. For example, you can’t demand an opioid if you have no pain condition, or an antibiotic for a virus. But within the range of suitable treatments, you have the right to choose based on your values, lifestyle, and preferences.
Can cost affect my right to choose?
Cost doesn’t remove your right to choose, but it can limit your options. If a drug is too expensive, your doctor should help you find alternatives, including generics, biosimilars, or patient assistance programs. You have the right to ask: “Is there a cheaper option that works just as well?” Many patients change or skip doses because of cost-but you shouldn’t have to. Speak up. Pharmacies and clinics often have resources you don’t know about.


Courtney Blake
December 11, 2025 AT 21:59This whole 'patient autonomy' thing is just woke medicine nonsense. Doctors know best. If I wanted advice from some guy on Reddit who can't even spell 'pharmacology', I'd go to TikTok. You don't get to pick your meds like they're Netflix shows. We're not in a democracy when it comes to antibiotics, folks.
Lisa Stringfellow
December 12, 2025 AT 10:03Ugh. Another article pretending patients are adults. My last doctor just handed me a script and said 'take this' while scrolling through his phone. I didn't even get to ask about side effects. And now you want me to 'ask questions'? Like I have time to become a medical expert between daycare drop-off and my second job. This is exhausting.
Monica Evan
December 12, 2025 AT 19:16As someone who's been on 7 different meds for chronic migraines, I can tell you this: autonomy saved my life. My first doc prescribed topiramate and said 'it's the gold standard.' I asked about weight gain, brain fog, and cost. He shrugged. I switched. New doc sat down with me for 45 mins, showed me a chart comparing options, even had me try a non-drug biofeedback app first. I'm now on a cheaper generic that doesn't make me feel like a zombie. And yes, I cried. Not because I was sad - because someone finally treated me like a human. You don't need a PhD to know what your body feels. Just ask. And if they roll their eyes? Find a new doctor. You deserve better.
Jean Claude de La Ronde
December 12, 2025 AT 22:41So let me get this straight - we’ve gone from 'doctor knows best' to 'patient is the CEO of their own body' and now we’re all supposed to be little pharmacists with a Google account? Brilliant. Next they’ll let me decide if my liver needs a vacation. At least back in the 80s, doctors were arrogant but competent. Now? We’ve got people asking if their antidepressant should be taken with oat milk. Autonomy? More like chaos with a wellness influencer filter.
Jim Irish
December 13, 2025 AT 18:54Shared decision-making works. The data is clear. Patients who understand their options adhere better. That’s not theory. It’s clinical reality. The challenge is time and training. Most doctors want to do this. They’re just drowning in paperwork and 15-minute slots. We need systemic change - not just patient pressure.
Mia Kingsley
December 14, 2025 AT 13:47OMG I JUST HAD THIS EXACT THING HAPPEN. My doctor gave me a script for gabapentin for nerve pain and I said 'wait, isn't that the one that makes you gain 20 lbs and feel like a zombie?' He said 'oh no, that's just for old people.' I looked it up. He was WRONG. I refused. He got mad. I left. Now I'm on pregabalin and I'm not crying every night. Don't trust your doctor. Trust yourself. And Google. Always Google.
Katherine Liu-Bevan
December 16, 2025 AT 00:31One thing missing from this article: language access. I work in a clinic where 40% of patients speak Spanish as their first language. Many aren’t given translated materials. They nod along because they don’t want to seem difficult. Autonomy isn’t possible without true comprehension. Translation services aren’t a luxury - they’re a necessity. And they’re underfunded. This isn’t just about asking questions - it’s about making sure people can understand the answers.
Vivian Amadi
December 16, 2025 AT 16:11YOU HAVE NO RIGHT TO REFUSE MEDS. YOUR DOCTOR IS A PROFESSIONAL. YOU’RE NOT A CHILD WHO GETS TO PICK ICE CREAM FLAVOR. THIS ISN’T A TIKTOK TRENDS VIDEO. PEOPLE ARE DYING BECAUSE THEY’RE LISTENING TO REDDIT INSTEAD OF DOCTORS. STOP BEING SO SELF-ENTITLED. TAKE YOUR PILLS.
Aidan Stacey
December 18, 2025 AT 04:49I’m a nurse who’s seen both sides. I’ve watched patients die because they didn’t understand their meds. I’ve also watched them thrive because they were heard. This isn’t about being 'difficult' - it’s about being human. If your doctor treats you like a number, find one who treats you like a person. You’re not asking too much. You’re asking for what you’ve always deserved.
Kristi Pope
December 18, 2025 AT 20:24Love this. I used to be the quiet one who just took whatever was handed to me. Then my dad had a bad reaction to a drug they didn’t even tell him about. After that, I started asking the five questions in the article. Changed everything. Now I help my friends do the same. It’s not about being an expert - it’s about being prepared. And yeah, sometimes I say 'I need to think about it.' And guess what? My doctor always says 'good.' That’s the sign of a real partner.
Aman deep
December 20, 2025 AT 06:25Coming from India where doctors still sometimes hand out scripts without a word, this hit home. I had to travel to the US to learn that asking 'why?' isn't rude - it's smart. Here, my doctor showed me a chart comparing costs and side effects. In India? I got a scrip and a pat on the head. But I’m bringing this home. Telling my cousins to ask. Teaching my sister to read the leaflet. Autonomy isn’t Western - it’s human.