Medication Safety Checker
Medication Safety Assessment
This tool helps you identify medications that may be inappropriate for older adults based on evidence-based guidelines like the Beers Criteria and STOPP/START. Review your current medications to see which ones might be candidates for deprescribing.
Every year, millions of older adults take more medications than they need. Some have been on the same pills for decades-antacids for occasional heartburn, sleeping pills for restless nights, or antipsychotics for mild agitation. But what if those medications are doing more harm than good? That’s where deprescribing comes in. It’s not about stopping meds cold turkey. It’s a careful, step-by-step process to remove drugs that no longer serve you, especially when the risks outweigh the benefits.
What Exactly Is Deprescribing?
Deprescribing is the planned, gradual reduction or discontinuation of medications that may no longer be necessary-or that might be causing more harm than help. It’s not a one-size-fits-all approach. It’s personalized. You look at the patient’s age, health goals, life expectancy, and what matters most to them. Is it living independently? Avoiding falls? Sleeping through the night? Reducing confusion? It’s especially important for older adults. Around 40% of people over 65 take five or more medications at once-a situation called polypharmacy. And that’s where things get risky. Studies show that inappropriate polypharmacy contributes to nearly 30% of hospital admissions in this age group. Many of those admissions are preventable. The idea gained traction around 2010, led by researchers in Canada like Barbara Farrell and Cara Tannenbaum. Today, deprescribing.org is the go-to resource for evidence-based guidelines. And it’s not just a theory. Real-world trials show it works. One 2023 study with 372 older adults found that those who went through a structured deprescribing program ended up taking 1.6 to 1.8 fewer medications-without an increase in hospital visits or side effects.Which Medications Are Most Often Targeted?
Not all drugs are equal when it comes to deprescribing. Some carry higher risks, especially for older adults. Five medication classes are the main focus of current guidelines:- Proton-pump inhibitors (PPIs) - Often prescribed for heartburn, but many people stay on them years longer than needed. Long-term use can lead to nutrient deficiencies, bone fractures, and kidney issues.
- Benzodiazepines and sleep aids - Used for anxiety or insomnia, but they increase fall risk, confusion, and dependence. Tapering them slowly can improve alertness and balance.
- Antipsychotics - Sometimes given for behavioral symptoms in dementia, even though they’re not approved for that use. They raise the risk of stroke and sudden death in older adults with dementia.
- Antihyperglycemics - Blood sugar drugs like sulfonylureas can cause dangerous low blood sugar episodes in seniors, especially those with limited life expectancy.
- Opioid analgesics - Pain meds that can lead to addiction, constipation, dizziness, and breathing problems. Often overused for chronic, non-cancer pain.
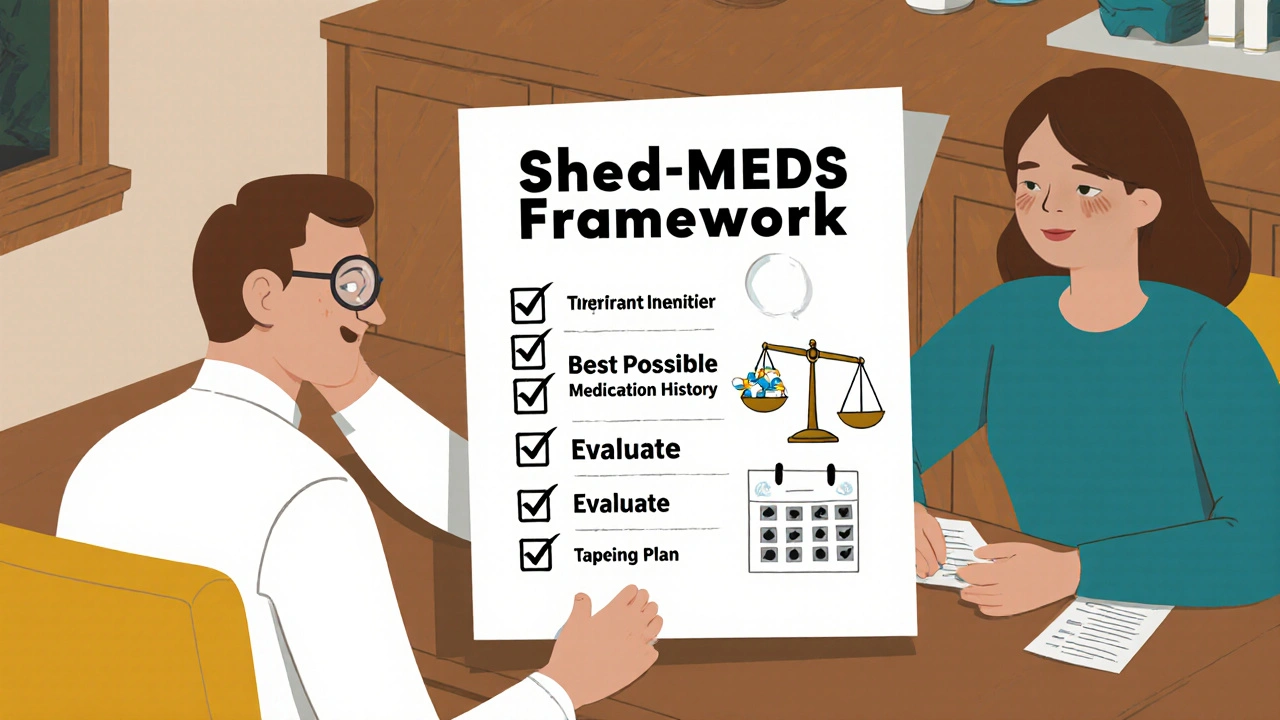
How Do You Actually Do It? The Shed-MEDS Framework
One of the most proven methods is called Shed-MEDS. It’s a simple four-step process used in hospitals and clinics across North America:- Best Possible Medication History - Get a complete list of everything the patient is taking, including over-the-counter pills, supplements, and creams. Many people forget to mention these.
- Evaluate - Use tools like the STOPP/START criteria (updated in 2021) or the Beers Criteria (2023 edition) to flag potentially inappropriate drugs. Ask: Is this drug still helping? Is it causing side effects? Does the patient’s condition still justify it?
- Deprescribing Recommendations - Decide which meds to stop or reduce. Prioritize high-risk drugs first. Always involve the patient. Don’t assume they want to stop everything.
- Synthesis - Create a clear plan: which drug to stop, how fast, what to watch for, and when to follow up. Give the patient a written schedule.
Why Isn’t Everyone Doing This?
If deprescribing works so well, why isn’t it standard practice? The biggest barrier? Time. Primary care doctors in the U.S. average just 7.2 minutes per patient visit. That’s not enough to review a list of 10+ medications, talk through risks and benefits, and build trust around stopping something the patient has taken for 15 years. Another issue? Lack of support. Only 32% of clinicians feel their electronic health records help them identify drugs to deprescribe. Most systems are built to remind doctors to prescribe-never to stop. And there’s fear. Both from doctors and patients. Doctors worry about being blamed if something goes wrong. Patients worry they’ll lose control or wake up feeling worse. A 2022 study found 22% of older adults felt anxious about stopping long-term meds-even when told it was safe. The good news? Pharmacists are making a huge difference. When pharmacists lead the process, deprescribing success rates jump by 35-40%. They have the training, the time, and the tools. In Canada, where pharmacist-led deprescribing is embedded in the system, 63% of primary care practices have formal protocols. In the U.S., it’s only 28%.What’s Changing in 2025?
Things are shifting fast. In June 2024, the American Medical Association issued its first official policy: physicians must routinely assess whether every medication is still appropriate. That’s huge. Medicare is catching up too. Starting in 2026, Medicare Advantage plans will be scored on how well they reduce inappropriate prescribing. That means hospitals and clinics will be financially incentivized to deprescribe. The National Institutes of Health is funding new research to create guidelines for 8 more drug classes-like antidepressants and blood thinners-that currently lack clear deprescribing pathways. AI tools are also being developed to scan electronic records and flag patients who might benefit from deprescribing. By 2030, experts predict deprescribing checks will be as routine as checking blood pressure during annual wellness visits. The goal? A 40% drop in medication-related hospitalizations among older adults by then.
What Patients Should Know
If you or a loved one is on multiple medications, here’s what to do:- Ask your doctor: “Is this medicine still helping? Could it be causing problems?”
- Bring a full list of everything you take-including vitamins, herbs, and OTC pills.
- Don’t stop anything on your own. Tapering matters. Stopping benzodiazepines or antidepressants too fast can cause seizures or rebound anxiety.
- Ask if a pharmacist can help review your meds. Many pharmacies offer free medication reviews.
- Track how you feel after a medication is reduced. Did your energy improve? Did the dizziness go away? Did you sleep better?
Tools and Resources You Can Use
You don’t need to figure this out alone. These are free, evidence-based tools used by professionals:- deprescribing.org - Offers downloadable algorithms for tapering PPIs, benzodiazepines, antipsychotics, and more.
- STOPP/START Criteria (v3, 2021) - A checklist that tells you which drugs to avoid and which to start in older adults.
- Beers Criteria (2023) - The gold standard list of potentially inappropriate medications for seniors.
Final Thought: It’s Not Just Stopping-It’s Starting Over
Deprescribing isn’t the opposite of prescribing. It’s just as intentional. You don’t just take a pill off the list. You replace it with safety, clarity, and quality of life. For many older adults, reducing medications means more energy, fewer trips to the bathroom at night, less dizziness when standing up, and the ability to enjoy meals with family without worrying about pill schedules. It’s not about taking fewer pills. It’s about living more.Is deprescribing safe?
Yes, when done properly. Multiple studies, including a 2023 JAMA Internal Medicine trial with 372 older adults, show no increase in hospitalizations or deaths when medications are reduced using structured deprescribing protocols. The key is gradual tapering and close monitoring-not sudden stops.
Can I stop my medications on my own?
No. Some medications, like benzodiazepines, antidepressants, and blood pressure drugs, can cause serious withdrawal symptoms if stopped abruptly. Always work with your doctor or pharmacist to create a safe tapering plan.
Who should consider deprescribing?
Anyone taking five or more medications, especially older adults, those with limited life expectancy, or those experiencing side effects like dizziness, confusion, falls, or fatigue. It’s also important for people whose health goals have changed-for example, shifting from disease prevention to comfort and quality of life.
Do deprescribing guidelines apply to younger people?
While most guidelines focus on older adults, the principles apply to anyone on long-term medications with unclear benefits. For example, people on PPIs for years without a confirmed diagnosis, or those on opioids for chronic non-cancer pain, can benefit from deprescribing regardless of age.
How long does it take to deprescribe?
It varies. For some drugs, like PPIs, tapering takes 4-8 weeks. For benzodiazepines, it can take 3-6 months. The pace depends on the drug, the person’s health, and how they respond. Patience and monitoring are key.
Will I feel worse after stopping meds?
Some people experience temporary symptoms as their body adjusts-like rebound heartburn or mild anxiety. But these usually fade within days or weeks. Many report feeling better overall: more alert, less groggy, fewer side effects. Tracking symptoms during the process helps distinguish true withdrawal from improved well-being.
What if my doctor doesn’t know about deprescribing?
Bring printed guidelines from deprescribing.org or the Beers Criteria. Ask if a pharmacist can help review your meds. Many pharmacies offer free medication reviews. You can also request a referral to a geriatrician or clinical pharmacist specializing in medication management.


Oyejobi Olufemi
November 16, 2025 AT 06:19Let me tell you something-this whole deprescribing movement is just Big Pharma’s backdoor to kill off geriatric care! They’ve been pushing these pills for decades, now they want you to believe it’s safe to stop? Ha! The FDA’s been compromised since 2012, and you think they’d let a protocol like this pass without a hidden agenda? I’ve seen the leaked memos-pharmaceutical reps are quietly incentivizing doctors to deprescribe so they can sell the ‘next-gen’ alternatives at triple the price. Wake up, people!
Teresa Smith
November 17, 2025 AT 08:33While I appreciate the intent behind deprescribing, the implementation is where things get messy. Many elderly patients have been on these medications for years-not because they were prescribed blindly, but because they’ve tried everything else. The emotional weight of letting go of something that’s kept you stable for a decade is not trivial. A compassionate, patient-led approach is essential. The data is promising, yes-but numbers don’t feel dizziness or panic attacks. We need more than protocols; we need presence.
ZAK SCHADER
November 18, 2025 AT 22:34Deprescribing? Sounds like another liberal health fad. My dad took his blood pressure med for 20 years and still walks 5 miles a day. You want to take that away? For what? To save a few bucks? The system is broke, not the meds. And dont even get me started on pharmacists running the show. We dont need pharmacy techs playing doctor. Let the MDs decide. End of story.
Daniel Stewart
November 20, 2025 AT 02:04There’s a profound metaphysical irony here: we’ve constructed an entire medical edifice on the assumption that more intervention equals better outcomes. Yet, the body-wise, ancient, and self-regulating-has spent millennia adapting to fewer chemicals, not more. Deprescribing, then, isn’t medicine’s evolution-it’s its homecoming. We’ve mistaken the map for the territory, the pill for the peace. Perhaps the real treatment was never in the bottle, but in the quiet, unmedicated silence between heartbeats.
Latrisha M.
November 21, 2025 AT 21:59My mother went through deprescribing last year. She was on seven meds, including a PPI she’d been on since 2008. After tapering, her energy improved, her balance got better, and she stopped falling in the bathroom. She didn’t feel worse-she felt like herself again. The key was a pharmacist who listened, a slow taper, and weekly check-ins. It’s not magic. It’s medicine done right.
Jamie Watts
November 22, 2025 AT 02:16Look I’ve been doing this for years and I know what works. If you’re on more than 5 meds you’re already a walking disaster. Stop being scared. Just quit the stupid pills. I got my uncle off 11 meds in 3 weeks and he’s hiking now. You dont need a whole framework. You need guts. The doctors are scared because they’re used to writing scripts not thinking. The system is broken and you need to break it yourself. Trust me I know.
John Mwalwala
November 22, 2025 AT 09:02Did you know that the deprescribing guidelines were secretly drafted by a shadow consortium linked to the World Health Organization’s Project Bluebeam? They’re trying to depopulate the elderly through ‘medication reduction’ under the guise of safety. The Beers Criteria? A front. The real goal is to make seniors dependent on wearable biomonitors and AI-driven health dashboards. That’s why they’re pushing pharmacists-they’re the new data harvesters. Watch your vitals next time you go in for a med review. You’re being tracked.
Deepak Mishra
November 22, 2025 AT 21:33OMG I JUST READ THIS AND I CRIED 😭 My grandma took 14 pills a day and she was always so tired… we started deprescribing last month and now she’s baking cookies again 🍪💖 I cant believe we waited so long! Thank you for writing this!! I printed the Beers Criteria and showed my doctor and he was like ‘huh’ and then he actually listened!! #DeprescribingIsLifeChanging
Rachel Wusowicz
November 23, 2025 AT 14:38They say it’s safe-but who’s really monitoring? The 1.8 fewer pills? That’s a statistic. What about the 12-year-old woman in Ohio who died after her psychiatrist abruptly pulled her SSRIs because of a ‘cost-saving initiative’? That wasn’t deprescribing. That was a murder disguised as policy. And now they’re pushing AI to automate this? You’re handing death decisions to an algorithm trained on insurance claims. I’ve seen the code. It flags the elderly as ‘low value.’ This isn’t medicine. It’s eugenics with a wellness aesthetic.
Diane Tomaszewski
November 24, 2025 AT 02:11I’ve seen this work in my own family. My dad stopped his sleeping pills after a year of slow tapering. He didn’t get worse-he got better. He started reading again. He laughed more. The meds weren’t helping. They were just noise. Sometimes less really is more. It’s not about being anti-pill. It’s about being pro-life.
Dan Angles
November 24, 2025 AT 07:27As a geriatric care coordinator, I can confirm that structured deprescribing, when implemented with interdisciplinary collaboration and patient-centered communication, consistently improves functional outcomes and reduces adverse events. The Shed-MEDS framework, supported by updated STOPP/START criteria and pharmacist integration, represents a paradigm shift in clinical practice. Institutional barriers remain significant, but policy changes such as Medicare’s 2026 incentive structure and AMA’s 2024 policy directive are catalyzing systemic adoption. The data is unequivocal: deprescribing saves lives, not just costs.