Anticoagulant Spinal Procedure Calculator
Key Safety Information
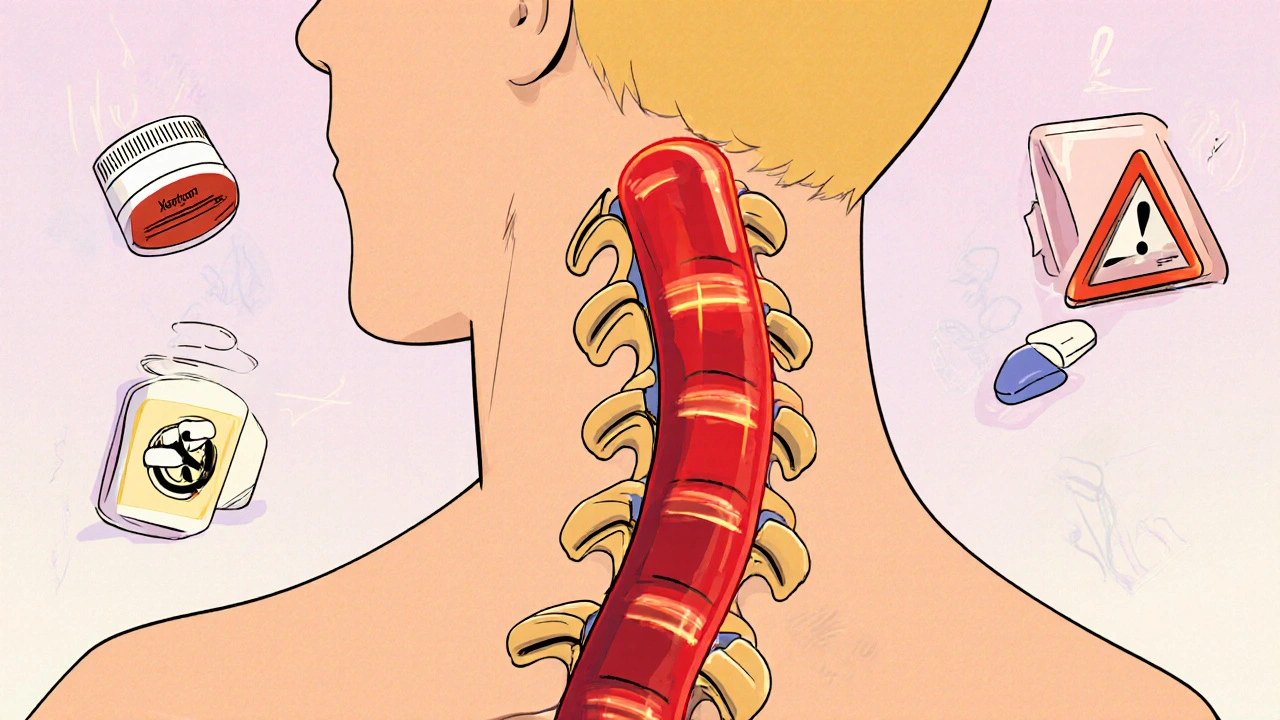
When you're on blood thinners and need an epidural or spinal procedure-whether for labor, back pain, or surgery-the last thing you want is a rare but devastating complication: a spinal hematoma. It’s not common, but when it happens, it can change your life forever. A hematoma in the spinal canal can crush the spinal cord, leading to paralysis, loss of bladder control, or even death. And the risk doesn’t go away just because you feel fine. It’s hidden in timing, medication type, and how your body responds.
What Exactly Is a Spinal Epidural Hematoma?
A spinal epidural hematoma (SEH) is a collection of blood that forms between the dura (the tough outer membrane around your spinal cord) and the bones of your spine. It doesn’t take much-just 1 to 2 milliliters of blood-to compress the spinal cord because the space is so tight. This isn’t like a bruise on your skin. Inside your spine, there’s no room to expand. The pressure builds fast, and nerves start dying within hours. Symptoms don’t wait. Most people feel intense back pain right away-93% do. Then comes numbness, weakness in the legs, or trouble peeing or pooping. If you’ve had a procedure and these show up within 12 hours, it’s an emergency. Studies show that if you get surgery within 8 hours, there’s a 79% chance you’ll fully recover. Wait past 24 hours, and that drops to 9%. Time isn’t just important-it’s everything.Which Blood Thinners Are Most Dangerous?
Not all anticoagulants are created equal. The risk depends on the drug, the dose, and how long it’s been since your last dose. Warfarin is the old-school blood thinner. If your INR (a blood test that measures clotting time) is above 1.4, your risk jumps 8.7 times compared to someone with normal clotting. Even if your INR is normal, there are cases where people still developed hematomas. That’s why guidelines say: check your INR within 24 hours before the procedure and make sure it’s below 1.4. Low Molecular Weight Heparin (LMWH) like Lovenox is used often after surgery to prevent clots. But here’s the catch: if you take a therapeutic dose (the kind used to treat clots, not just prevent them) and have the procedure within 10 to 12 hours, your risk is 0.31%. Wait 24 hours, and it drops to 0.04%. That’s a huge difference. Many hospitals now require holding LMWH for 24 hours before spinal procedures-especially if you’re getting a catheter placed. Direct Oral Anticoagulants (DOACs) like rivaroxaban (Xarelto), apixaban (Eliquis), and dabigatran are newer and easier to manage-but still risky. Rivaroxaban carries a 0.08% risk if stopped 48 hours before, but that jumps to 0.42% if stopped too late. Apixaban is slightly safer at 0.05%. But if you have kidney problems (CrCl under 50 mL/min), you need to stop it for 72 hours instead. Why? Because your body can’t clear the drug fast enough. The guidelines are precise: 48 hours for normal kidneys, 72 for impaired ones.It’s Not Just the Drug-It’s the Procedure Too
The type of procedure matters just as much as the medication. A simple lumbar puncture for a spinal fluid test has a risk of just 0.001%. An epidural steroid injection for back pain? About 1 in 15,000. But if you’re having a complex spine surgery with multiple levels or an epidural catheter left in place? That risk climbs to 0.5% to 1.0%. Why? Because each time the needle goes in, it can nick a blood vessel. Three or more needle passes? Risk goes up 6.2 times. If the fluid that comes out is tinged with blood? That’s a red flag-risk jumps 11.8 times. And leaving a catheter in? That’s 2.3 times more dangerous than a single shot. Even the patient’s body plays a role. Age over 70? Risk triples. Kidney disease? Risk nearly five times higher. Spinal stenosis? Risk doubles. If you’re anemic (hemoglobin under 10 g/dL) or lost more than a liter of blood during surgery? You’re in a higher-risk group too.What About Aspirin and Other Antiplatelets?
This is where things get messy. Aspirin alone? Most studies show almost no increased risk. One study of over 1,200 patients who kept taking aspirin before epidural injections had zero hematomas. Another study of 101 procedures with aspirin showed no complications. So if you’re on aspirin for heart protection, you probably don’t need to stop. But dual antiplatelet therapy? That’s different. If you’re taking both aspirin and clopidogrel (Plavix)-common after stents or heart attacks-your risk goes up 3.8 times. Some doctors say stop both for 7 days. Others say 5. But the evidence is clear: don’t take both into a spinal procedure unless absolutely necessary. There’s disagreement among experts. One group says aspirin is fine. Another says even a single antiplatelet can be dangerous in high-risk patients. The bottom line? Don’t assume. Talk to your anesthesiologist. Bring your pill bottle. Let them know exactly what you’re taking and why.Timing Is Everything-Here’s the Real Schedule
Forget vague advice like “stop your blood thinner.” You need exact hours.- Warfarin: Check INR within 24 hours before. Target: <1.4. Restart 4 hours after single injection, 6 hours after catheter.
- LMWH (prophylactic dose): Hold for 10-12 hours before. Restart 2 hours after single injection, 4 hours after catheter.
- LMWH (therapeutic dose): Hold for 24 hours before. Restart 2-4 hours after, depending on catheter.
- Rivaroxaban (Xarelto): Stop 48 hours before (72 if kidney issues). Restart 6-24 hours after, depending on bleeding risk.
- Apixaban (Eliquis): Stop 48 hours before (72 if kidney issues). Restart 6-24 hours after.
- Dabigatran: Stop 48 hours before (72 if kidney issues). Restart 6-24 hours after.
What Happens If You Ignore the Rules?
The consequences aren’t theoretical. In 2013, the FDA reviewed 170 cases linked to Lovenox. 100 were confirmed. Many patients were told it was “safe” because they were on prophylactic doses. They weren’t. One case: a 68-year-old man had hip surgery, got an epidural catheter, and was on rivaroxaban. He was told to stop 48 hours before. He didn’t. Twelve hours after the catheter was removed, he lost feeling in his saddle area. Emergency surgery happened-but he still lost permanent nerve function in his L5 nerve. He now uses a wheelchair. Another: a woman on warfarin had an INR of 1.2 before an epidural. Normal. But she developed a hematoma anyway. Surgery within 6 hours. She still ended up with permanent foot drop. These aren’t outliers. They’re textbook cases of what happens when timing is off, documentation is poor, or assumptions are made.
How Do You Stay Safe?
You’re not powerless. Here’s what you can do:- Bring a list: Write down every medication, including supplements and over-the-counter pills. Don’t rely on memory.
- Ask questions: “What’s my risk? What’s the plan if something goes wrong?”
- Confirm timing: Don’t assume your doctor knows the guidelines. Ask: “When exactly should I stop my blood thinner? When can I restart?”
- Know the symptoms: Back pain, leg weakness, numbness, trouble urinating-call 911 or go to the ER immediately if they appear after a spinal procedure.
- Use tools: Apps like “Neuraxial Anticoag” are updated quarterly and help doctors follow guidelines. Ask if your provider uses them.

Amie Wilde
November 12, 2025 AT 13:44Just had an epidural last month on apixaban. Stopped it 48 hours before like the doc said. Felt fine. But man, the anxiety was real. I kept checking my legs every 10 minutes. Don't even get me started on the nurse asking me 3 times if I was sure I didn't take my pill the day before.
Gary Hattis
November 13, 2025 AT 08:27As a former ER nurse in Texas, I’ve seen too many of these. One guy came in paralyzed after a back injection-he was on Xarelto, thought "it’s just a little shot." Didn’t stop it. Family sued. Hospital lost. Docs need to stop assuming patients know what they’re on. Bring your pill bottles. No excuses.
Esperanza Decor
November 13, 2025 AT 13:06My mom had a spinal fusion last year. She was on warfarin. They checked her INR three times before the procedure. One nurse even printed out the ASRA guidelines and went over them with her. That’s the kind of care you want. Not the "oh, you’re on blood thinners? We’ll wing it" stuff. Knowledge saves spines.
Deepa Lakshminarasimhan
November 13, 2025 AT 13:22They say it’s rare. But why do all the big hospitals use the same protocols? Why is the FDA pushing new rules? Why are women getting it 2.3x more? Coincidence? Or are they hiding something? I’ve seen how pharma pushes drugs without full safety data. This feels like another cover-up. Ask yourself-why aren’t they testing everyone’s spinal fluid after these procedures?
Erica Cruz
November 13, 2025 AT 22:20Wow. So much information. So little actual science. 0.08% risk? That’s like saying you’re more likely to be struck by lightning while winning the lottery. People are panicking over numbers that barely register on the risk radar. Meanwhile, we’re overmedicating everyone and calling it "safety."
Johnson Abraham
November 15, 2025 AT 05:22lol so if u on xarelto u gotta wait 48hrs? what if u r 70 and got kidney issues? 72hrs? bruh. i just take my pills and hope for the best. also why is it always "women get it more"? maybe they just complain more? 🤷♂️
Shante Ajadeen
November 15, 2025 AT 06:26This was so helpful. I’ve been on aspirin for my heart and was scared to get my epidural for sciatica. Now I know it’s probably fine. Thank you for breaking it down without the fearmongering. Seriously, if you’re on meds like this, print this out and take it to your appointment. It’s your body-ask the questions.
dace yates
November 15, 2025 AT 15:15Does anyone know if the GFAP blood test is available outside of research hospitals yet? I’m curious if it’s being used in community clinics or if this is still just a paper thing.
Danae Miley
November 15, 2025 AT 16:52Correction: The 2024 ASRA draft guidelines do not use a "score over 15" threshold-this is a misinterpretation. The actual tool is a risk stratification matrix with categories: low, moderate, high, and very high. The threshold for "very high" is a composite of ≥4 risk factors, not a numeric score. Please don’t spread misinformation.
Charles Lewis
November 17, 2025 AT 15:22It’s worth emphasizing that the real issue isn’t just the pharmacokinetics of anticoagulants-it’s systemic. In many outpatient pain clinics, there is no dedicated anesthesiologist on-site. Nurses are expected to interpret complex guidelines without formal training. The 42% statistic isn’t just about ignorance-it’s about under-resourcing. Until we invest in procedural safety infrastructure, no amount of patient education will prevent tragedies. This isn’t a patient problem. It’s a healthcare system failure.
Renee Ruth
November 18, 2025 AT 21:51My cousin lost her ability to walk after an epidural. They said it was "rare." But she was on Lovenox. They told her it was "prophylactic." She was 62. She had stenosis. She was anemic. And they still did it. Now she’s in a wheelchair. And the hospital settled out of court. No one was fired. No one apologized. Just another statistic. Don’t trust them. They don’t care until it’s too late.