Swallowing seems simple-until it doesn’t. If you’ve ever felt food stick in your chest, had trouble getting liquids down, or experienced chest pain that feels like a heart attack, you might be dealing with something more serious than indigestion. These symptoms often point to esophageal motility disorders, conditions where the muscles of the esophagus don’t work the way they should. Unlike GERD, where stomach acid backs up, these disorders are about movement-specifically, the failure of coordinated muscle contractions to push food into the stomach.
What Exactly Is Happening in the Esophagus?
Your esophagus isn’t just a passive tube. It’s a muscular pipeline that contracts in a wave-like motion called peristalsis. Think of it like squeezing a toothpaste tube from the bottom up-each contraction pushes food forward. In esophageal motility disorders, this wave breaks down. Sometimes it’s too weak. Sometimes it’s too strong. Sometimes it happens in the wrong order. The result? Food lingers, gets stuck, or even comes back up.The most common symptom is dysphagia-difficulty swallowing. It usually starts with solids, then progresses to liquids. People often describe it as food "sticking" or "pausing" behind the breastbone. Other signs include regurgitation of undigested food, chest pain, and unintentional weight loss. Surprisingly, many patients are misdiagnosed with acid reflux for years. They take proton pump inhibitors (PPIs) daily, but nothing changes because the problem isn’t acid-it’s muscle function.
How Do Doctors Know It’s Not Just GERD?
The first step is usually an upper endoscopy. A camera is passed down the throat to check for blockages, inflammation, or tumors. If nothing’s found, the next step is esophageal manometry. This isn’t a scan or an X-ray. It’s a pressure test. A thin, flexible tube with sensors is inserted through the nose and into the esophagus. As you swallow sips of water, the sensors measure the strength, timing, and coordination of each muscle contraction.For decades, this was done with a single pressure sensor. Today, most hospitals use high-resolution manometry (HRM). It has 36 sensors spaced just 1 cm apart. That means doctors can see exactly where and how the esophagus is failing. The data creates a color-coded map-like a weather map showing pressure storms across the esophagus. This is how conditions like achalasia, nutcracker esophagus, and jackhammer esophagus are identified.
The Chicago Classification: A New Standard
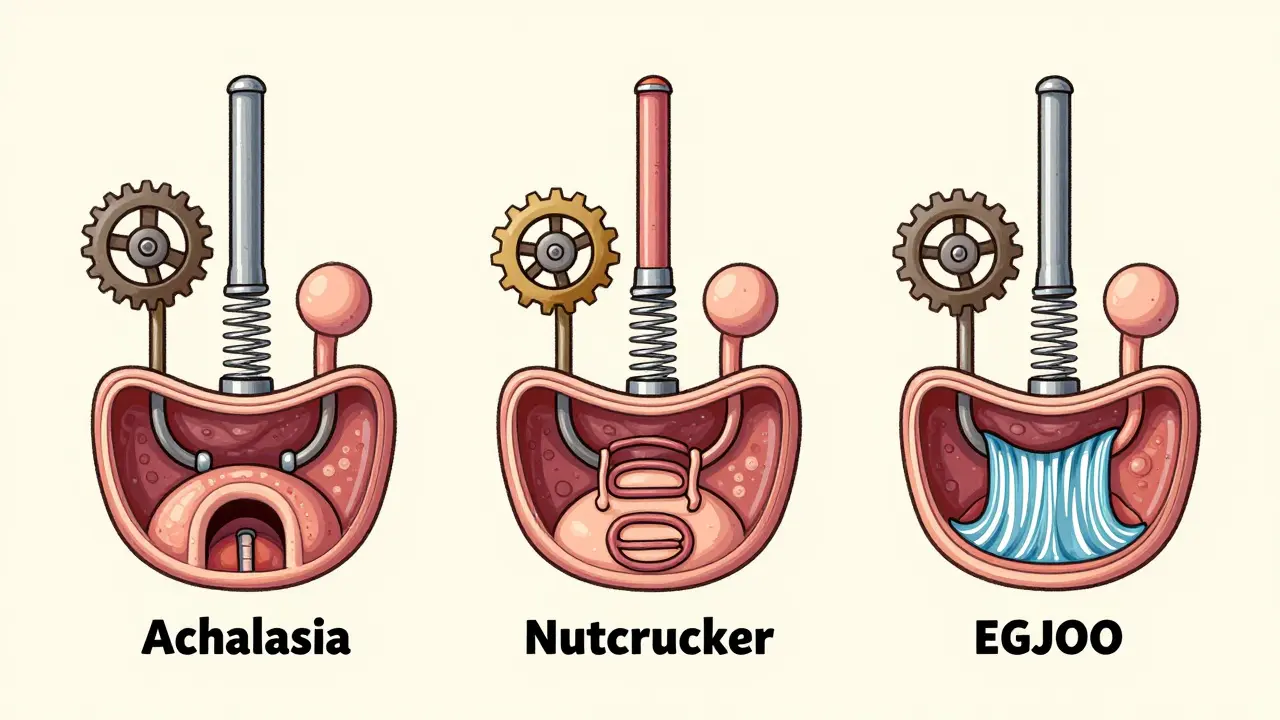
In 2023, the latest version of the Chicago Classification (v4.0) became the global standard for diagnosing these disorders. Before this, doctors often disagreed on what counted as "abnormal." Now, every major medical center uses the same criteria. For example:- Achalasia: The lower esophageal sphincter (LES) won’t relax. Peristalsis is absent or chaotic. It’s split into three types: Type I (no contractions), Type II (pan-esophageal pressurization), and Type III (spasms).
- Nutcracker esophagus: Contractions are strong-over 180 mmHg-but coordinated. Often causes chest pain.
- Jackhammer esophagus: Even stronger contractions, with a distal contractile integral over 5,000 mmHg•s•cm. This can feel like a heart attack.
- Esophagogastric junction outflow obstruction (EGJOO): The LES pressure is high, but peristalsis is normal. This is a newer category introduced in 2023.
These distinctions matter. Treatment changes based on the type. Mislabeling one as another can lead to ineffective or even harmful care.

Manometry vs. Other Tests
Barium swallow tests used to be common. You drink chalky liquid, and X-rays track its movement. But they miss up to 22% of motility disorders. HRM catches 96% of achalasia cases-far better than barium’s 78%. Another option, EndoFLIP, measures how stretchy the esophagus is. It’s useful for evaluating obstruction, especially in complex cases.But manometry isn’t perfect. The tube can be uncomfortable. About 35% of patients report moderate to severe discomfort. And it’s not available everywhere. Only 95% of academic hospitals in the U.S. have HRM. In rural areas or low-income countries, access is rare. That’s why some patients wait years for a diagnosis. One survey found 68% waited 2-5 years and saw at least three doctors before getting the right answer.
Treatment: One Size Doesn’t Fit All
Treatment depends entirely on the diagnosis.- Achalasia: The gold standard is surgery-laparoscopic Heller myotomy (LHM), where the tight LES muscle is cut. Success rates are 85-90% at five years. A newer option is POEM (peroral endoscopic myotomy), done entirely through the mouth. It’s equally effective but carries a higher risk of reflux-44% of patients develop esophagitis within two years.
- Pneumatic dilation: A balloon is inflated in the LES to stretch it. It works for 70-80% of patients initially, but 25-35% need repeat procedures within five years.
- Nutcracker and jackhammer: These are harder to treat. Calcium channel blockers or nitrates can help relax the muscle. Botox injections into the LES are sometimes used. In severe cases, surgery may be considered.
- Secondary disorders: If the cause is scleroderma, treatment focuses on the underlying disease. The esophagus may need dietary changes, medications, or even feeding tubes in advanced cases.
There are also emerging options. The LINX device, a magnetic ring implanted around the LES, is now being tested for select achalasia patients with preserved peristalsis. Early results show 75% symptom improvement at one year. And wireless capsules like the SmartPill let patients wear a tiny sensor for 24-48 hours, recording motility while they go about their day. It’s less invasive and correlates with HRM at 85% accuracy.
What Patients Say
Real stories highlight the gap between diagnosis and relief. One Reddit user wrote: "After my POEM, I ate a burger for the first time in seven years. I cried." Another shared on a health forum: "I was on PPIs for eight years. My doctor said I had GERD. Manometry revealed jackhammer esophagus. Everything changed after that."But not all experiences are positive. Some patients get labeled with "minor motility disorders"-abnormal patterns that may not even cause symptoms. Experts warn against overtreating these. As Dr. C. Prakash Gyawali put it: "We can’t treat every weird pressure wave. Many are just noise."
Why This Matters Now
The market for esophageal diagnostic tools is growing fast-projected to hit $410 million by 2028. More hospitals are investing in HRM. Fellowship programs now require motility training. AI tools are being trained to read manometry tracings with 92% accuracy, outperforming untrained humans. But access remains unequal. If you live outside a major city, getting tested might mean traveling hundreds of miles.The key takeaway? If you have persistent dysphagia, especially if PPIs don’t help, don’t accept "it’s just acid reflux." Ask for manometry. It’s the only test that shows how your esophagus actually moves. And with the Chicago Classification v4.0, doctors now have a clear roadmap to diagnose-and treat-these disorders accurately.
Can dysphagia be caused by something other than motility disorders?
Yes. Dysphagia can also stem from structural issues like esophageal strictures, tumors, or external compression from enlarged lymph nodes or thyroid glands. That’s why doctors start with an endoscopy-to rule out these problems before testing motility. If the esophagus looks normal, then motility disorders become the next focus.
Is high-resolution manometry painful?
It’s uncomfortable, but not usually painful. The tube is thin and lubricated. Most people feel pressure or a gag reflex when it’s inserted. Numbing spray helps. About 35% of patients report moderate discomfort, but only 5% say it’s unbearable. Breathing slowly and staying relaxed helps. The whole test takes about 20-30 minutes.
Can I have an esophageal motility disorder without having symptoms?
Rarely, but yes. Some people have abnormal manometry results with no swallowing problems. These are called "minor motility disorders" under the Chicago Classification v4.0. Experts now advise against treating these unless symptoms develop. Treating them unnecessarily can lead to complications from surgery or medications that aren’t needed.
How long does it take to get results from manometry?
The test itself takes less than an hour. But interpreting the data takes time. A trained specialist needs to analyze the pressure patterns, which can take several hours. Most clinics deliver results within 3-7 business days. If the case is complex or requires a second opinion, it may take longer.
Are there non-surgical treatments for achalasia?
Yes. Pneumatic dilation and botulinum toxin (Botox) injections are non-surgical options. Dilation stretches the LES and works well for many patients, though it may need repeating. Botox temporarily paralyzes the muscle, giving relief for 6-12 months. These are often used for older patients or those who can’t undergo surgery. But they’re not permanent fixes-surgery remains the most durable solution.