Gout Exercise Plan Calculator
This calculator helps you create a personalized exercise plan to lower uric acid levels and prevent gout flare-ups. Based on your current activity level, gout status, and preferences, it will recommend the most appropriate exercises and schedule for your needs.
Your Personalized Exercise Plan
Based on your inputs, here's the best exercise routine to help manage your gout while lowering uric acid levels.
Recommended Exercise
Weekly Frequency
Benefits for Your Situation
- Improved kidney function for better uric acid clearance
- Reduced risk of flare-ups
- Supports healthy weight management
- Enhanced joint mobility and flexibility
Important Considerations
Living with gout can feel like a constant battle against sudden, painful flare‑ups. While medication and diet get most of the spotlight, exercise plays a surprisingly powerful role in keeping uric‑acid levels in check and preventing attacks.
Key Takeaways
- Regular, moderate‑intensity activity helps the kidneys flush out excess uric acid.
- Low‑impact cardio, strength training, and flexibility work are the safest choices for gout sufferers.
- Consistency beats intensity - aim for at least 150 minutes a week.
- Stay hydrated, manage weight, and avoid joint‑stressing moves during flare‑ups.
- Combine exercise with a low‑purine diet for the best results.
Exercise is a physical activity that stimulates the body's systems, improves circulation, and promotes metabolic health. Regularly moving the body triggers a cascade of benefits that directly influence uric acid production and elimination.
Why Exercise Impacts Uric Acid
Uric acid is a waste product formed when the body breaks down purines-substances found in many foods and in our own cells. When levels climb too high, the crystal gout can develop, causing sudden joint pain, especially in the big toe.
Exercise helps in three measurable ways:
- Boosting kidney function. Moderate aerobic activity increases renal blood flow, allowing the kidneys to filter more uric acid from the blood.
- Promoting weight loss. Excess body fat is linked to higher uric‑acid production. Shedding pounds reduces the metabolic load and lowers serum urate.
- Reducing inflammation. Physical movement releases anti‑inflammatory cytokines, which can temper the fiery response that accompanies gout attacks.
Studies from 2023‑2024 show that participants who added 30 minutes of brisk walking five days a week saw an average 0.3mg/dL drop in serum uric acid after three months, compared to a control group with no change.
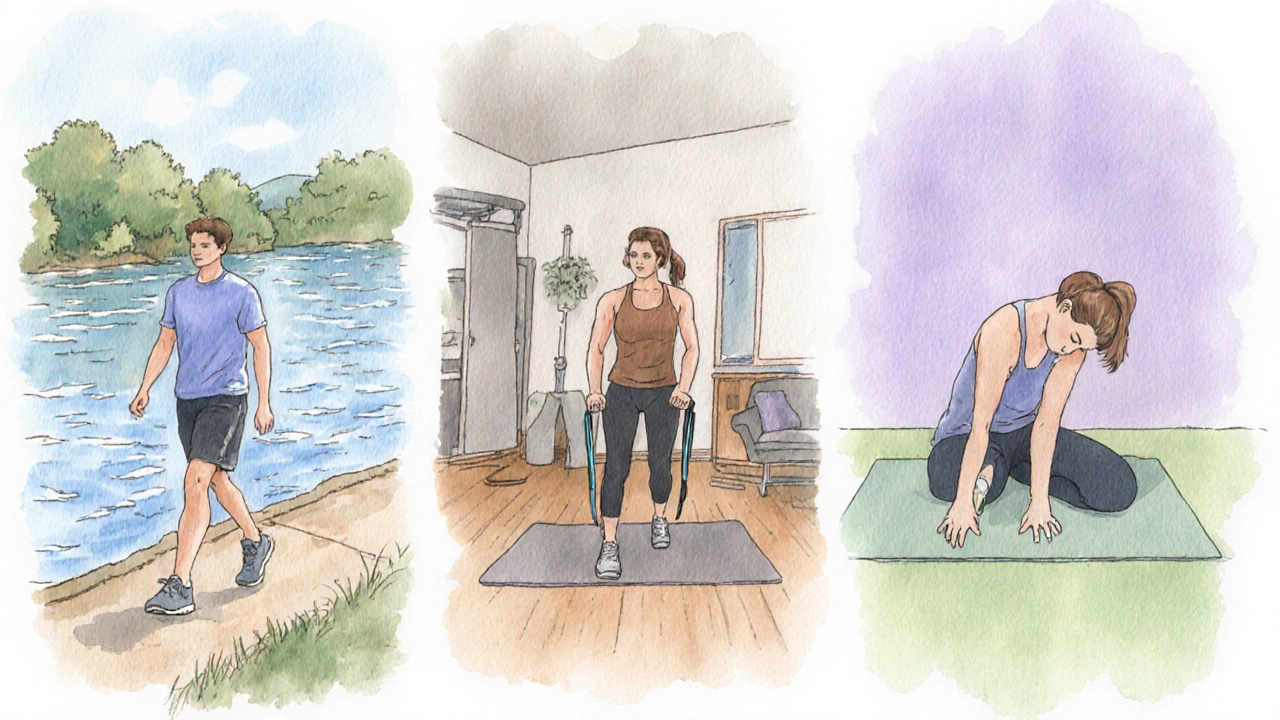
Best Types of Exercise for Gout
Not all workouts are created equal when it comes to gout. High‑impact or heavy‑load activities can stress inflamed joints, triggering pain. Here’s a quick guide to the safest and most effective options.
| Exercise | Impact Level | Uric‑Acid Effect | Frequency Recommendation | Best For |
|---|---|---|---|---|
| Low‑impact cardio (e.g., brisk walking, cycling) | Low | Improves kidney clearance; modest uric‑acid reduction | 30‑45min, 4‑5times/week | All stages, especially during flare‑ups |
| Strength training (machines, resistance bands) | Medium (if proper form) | Builds muscle, aids weight loss, indirect uric‑acid drop | 2‑3sessions/week, 20‑30min | Those aiming for long‑term weight control |
| Flexibility exercises (stretching, yoga) | Very low | Reduces joint stiffness; no direct uric‑acid impact but supports mobility | 10‑15min daily or post‑cardio | People with limited range of motion |
| High‑impact sports (running, basketball) | High | Can trigger flare‑ups due to joint stress | Avoid during active gout; replace with low‑impact options | Not recommended for gout management |
Building a Gout‑Friendly Weekly Plan
Below is a sample schedule that balances cardio, strength, and flexibility while keeping joint strain low. Adjust the timing to fit your lifestyle, but aim for at least 150 minutes of movement each week.
- Monday - Low‑impact cardio: 30‑minute brisk walk or stationary bike. Finish with 5‑minute gentle calf stretch.
- Tuesday - Strength: 20minutes of resistance‑band work targeting legs, back, and core. Keep reps moderate (12‑15) and avoid heavy loading on the knees.
- Wednesday - Flexibility + Rest: 15‑minute yoga flow focusing on hip and ankle mobility.
- Thursday - Low‑impact cardio: 35‑minute elliptical session at a steady pace.
- Friday - Strength: Body‑weight squat variations (avoid deep squats) and upper‑body push‑ups on a wall or bench.
- Saturday - Active recovery: Light swimming or a nature walk; keep intensity low.
- Sunday - Rest: Hydrate well, stretch lightly, and let the body recover.
Key points:
- Stay hydrated. Drinking at least 2‑3L of water daily helps the kidneys flush uric acid.
- Listen to your body - if a joint feels sore, switch to a gentler activity for that day.
- Combine workouts with a low‑purine diet (limit red meat, shellfish, and sugary drinks).
Common Pitfalls and Safety Tips
Even well‑intentioned exercise can backfire if you ignore a few basics:
- Skipping warm‑ups. Jumping straight into activity raises joint stress. Spend 5‑10minutes on light cardio and dynamic stretching.
- Overtraining. More isn’t always better. Pushing through pain can trigger a gout flare and cause injury.
- Ignoring dehydration. Sweat loss without fluid replacement concentrates uric acid, negating the kidney‑boosting benefits.
- Choosing high‑purine snacks post‑workout. Protein shakes loaded with whey concentrate can add purines; opt for plant‑based proteins instead.
- Neglecting footwear. Unsupportive shoes increase impact on the feet, a common gout hotspot.
When a flare‑up does occur, follow the "RICE" rule - Rest, Ice, Compression, Elevation - and keep activity light. Gentle range‑of‑motion exercises can prevent stiffness without aggravating pain.
Integrating Exercise with Overall Gout Management
Exercise is a piece of a larger puzzle that includes medication, diet, and lifestyle. Here’s how the pieces fit together:
- Medication synergy. Drugs like allopurinol lower uric‑acid production, while exercise improves clearance. Taking them together can reduce flare frequency.
- Dietary alignment. A diet low in purines (e.g., cherries, low‑fat dairy, whole grains) complements the uric‑acid‑lowering effect of regular activity.
- Weight management. Losing 5‑10% of body weight can cut serum urate by up to 0.5mg/dL, amplifying the benefits of exercise.
- Stress reduction. Physical activity releases endorphins, which help manage the emotional stress that can worsen gout symptoms.
By treating exercise as a daily habit rather than an occasional effort, you create a steady, supportive environment for all other treatments.
Frequently Asked Questions
Can I exercise during an active gout flare?
Yes, but keep the activity low‑intensity and short. Gentle walks or ankle circles can maintain circulation without overloading the inflamed joint. Stop immediately if pain worsens.
How soon will I see a drop in uric‑acid levels after starting to exercise?
Most people notice a modest reduction (0.2‑0.4mg/dL) after 8‑12weeks of consistent moderate cardio, especially when paired with proper hydration and diet.
Is strength training safe for gout?
Absolutely, as long as you avoid heavy loads on painful joints. Use machines or resistance bands, focus on controlled movements, and schedule strength sessions on days when joints feel okay.
How much water should I drink to help lower uric acid?
Aim for at least 2‑3liters (8‑12cups) a day. Increase intake during exercise or hot weather to compensate for sweat loss.
Should I avoid certain foods right after a workout?
Yes. Skip high‑purine items like red meat, organ meats, and certain seafood. Opt for a balanced post‑workout snack of low‑fat dairy, fruits, and whole‑grain carbs.


Albert Lopez
October 12, 2025 AT 19:53The pathophysiological nexus between aerobic conditioning and uric acid homeostasis merits rigorous scrutiny. Empirical investigations from the past quinquennium substantiate a modest yet reproducible decline in serum urate following sustained moderate-intensity exercise. Such outcomes derive principally from augmented renal plasma flow, which expedites glomerular filtration of purine metabolites. Moreover, the caloric deficit inherent in regular locomotion attenuates adipose-derived inflammatory cytokines implicated in urate elevation. It is incumbent upon clinicians to recognize that the therapeutic milieu for gout extends beyond pharmacologic agents. Conveying to patients the salutary impact of low‑impact cardio circumvents the iatrogenic reliance on urate‑lowering drugs alone. The literature further elucidates that resistance training, when calibrated to avoid excessive joint loading, contributes indirectly by fostering lean muscle mass. Increased musculature enhances basal metabolic rate, thereby diminishing endogenous purine turnover. Concomitant hydration, an oft‑overlooked element, synergizes with exercise to dilute serum uric concentrations. Practitioners should therefore prescribe a regimen encompassing at least 150 minutes of aerobic activity per week, supplemented by bi‑weekly strength sessions. Chronotropic moderation is advisable; target heart rates approximating 60‑70 % of age‑predicted maxima prove efficacious without precipitating gout flares. Patients experiencing acute attacks must temporarily eschew high‑impact modalities, favoring gentle ambulation or aquatic therapy. The temporal latency between exercise initiation and measurable urate reduction typically spans eight to twelve weeks, contingent upon adherence. It is prudent to monitor renal function periodically, given the heightened renal perfusion associated with sustained activity. In aggregate, these lifestyle interventions constitute a non‑pharmacological scaffold that can potentiate allopurinol or febuxostat therapy. Ultimately, the judicious integration of exercise into gout management epitomizes a holistic paradigm that aligns physiological benefit with patient empowerment.
Erica Harrington
October 20, 2025 AT 22:19Great rundown, Albert. I love how you broke down the science into actionable steps. Keep it up, everyone!
Patricia Mombourquette
October 28, 2025 AT 23:46exercise help gout but only if you dont overdo it
karl lewis
November 6, 2025 AT 02:13While the article commendably collates extant data, it neglects the philosophical dimension of bodily movement as a metaphor for existential agency. One could argue that the mere mechanistic reduction of gout to renal hemodynamics is an oversimplification of a complex biopsychosocial interplay. Moreover, the recommendation of “150 minutes per week” appears arbitrarily derived from generic guidelines rather than gout‑specific trials. The author fails to address the variability in individual metabolic phenotypes, which renders a one‑size‑fits‑all prescription dubious. In my view, a more nuanced protocol would tier intensity based on serum urate trajectories, not merely heart‑rate percentages. Nevertheless, the emphasis on hydration is a commendable nod to the often‑ignored fluid balance component. :)
Amy Martinez
November 14, 2025 AT 04:39Wow, Karl, you’ve turned a health tip into a philosophical odyssey! I love the vivid imagery-thinking of our muscles as tiny poets dancing away excess uric acid. Let’s keep the momentum rolling with those bright, rainbow‑colored walking shoes; they’re practically a passport to a gout‑free adventure. 🌈
Just Sarah
November 22, 2025 AT 07:06In consideration of the evidence presented, it is evident that regular, moderate‑intensity aerobic activity, complemented by judicious strength training, constitutes a cornerstone of gout prophylaxis; moreover, the synergistic effect of sustained hydration, calibrated caloric intake, and incremental progression, collectively, amplify renal urate clearance, thereby attenuating flare frequency, and promoting overall musculoskeletal resilience.
Anthony Cannon
November 30, 2025 AT 09:33Indeed, a balanced regimen yields optimal results.
Kristie Barnes
December 8, 2025 AT 11:59Sounds solid – I’ll start with short walks.
Zen Avendaño
December 16, 2025 AT 14:26I agree that consistency beats intensity, but it’s also vital to listen to your body’s signals. If a joint feels tender, swapping a run for a gentle bike ride can keep the routine alive without triggering a flare. Pairing these sessions with proper footwear and post‑exercise stretching helps maintain joint mobility. Remember, the goal is sustainable habit formation, not a sprint to perfection.
Christy Pogue
December 24, 2025 AT 16:53Exactly, Zen! Let’s keep the vibe positive and the steps steady – every little move adds up to big wins against gout.
Sunil Sharma
January 1, 2026 AT 19:19For anyone starting out, a good tip is to set a reminder on your phone for a 10‑minute walk after meals; it’s a simple way to integrate activity without feeling overwhelmed.
Steph Hooton
January 9, 2026 AT 21:46Thank you Sunil, that is a practical advice. I would also sugguest monitoring your uric acid levels every three months to gauge progress, as consistent data can motivate adherence to the plan.
Judson Voss
January 18, 2026 AT 00:13Honestly, this whole exercise‑gout narrative feels like a marketing buzzword salad. People will read the hype and ignore the fact that genetics play a far larger role than any jogging schedule.
Jessica Di Giannantonio
January 26, 2026 AT 02:39Oh, Judson, don’t let the shadow of doubt dim the sunrise of hope! A single stride can echo through our veins, turning the storm of uric acid into a calm sea of wellness.