Every year, millions of Americans rely on generic drugs to manage everything from high blood pressure to thyroid issues. They’re supposed to be cheaper-sometimes way cheaper-than brand-name pills. But if you’ve noticed your prescription cost jumping from $4 to $45 in a year, you’re not imagining it. Generic drug prices don’t move in a straight line. They spike, crash, and sometimes vanish entirely-year after year-with little warning.
Why Generic Drugs Are Supposed to Be Cheaper
Generic drugs contain the exact same active ingredients as brand-name drugs. They work the same way. They’re just sold without the marketing, the fancy packaging, or the patent protection. When a brand-name drug’s patent expires, other companies can make copies. More competitors usually mean lower prices. That’s the theory, anyway. In reality, the savings aren’t always steady. In 2022, generics made up 90% of all prescriptions filled in the U.S., but only 23% of total drug spending. That sounds great-until you realize that a small number of generics are driving up costs for everyone else. While most generics stay stable, about 15% see wild swings-some jumping over 100%, even 500% in a single year.How Competition Drives Prices Down (When It Works)
Price drops happen fast when multiple companies start making the same generic. The FDA found that when the first generic hits the market, prices often fall by 90% within a year. Add a second manufacturer? Prices drop another 25%. By the time you have four or more companies making the drug, prices can be as low as 15% of the original brand-name cost. For example, generic levothyroxine (used for hypothyroidism) dropped 87% between 2013 and 2018 because dozens of manufacturers entered the market. But that’s not the whole story.The Dark Side: When Fewer Companies Mean Higher Prices
Here’s where things get ugly. When only one or two companies make a generic drug, prices don’t fall-they rise. And they can rise fast. In 2013-2014, 8.2% of generic prescriptions saw price hikes between 100% and 500%. A single pill of nitrofurantoin (a common antibiotic) jumped 1,272% over five years. Why? Because the manufacturers that made it either shut down, got bought out, or stopped producing it. Suddenly, only one company was left. No competition. No pressure to lower prices. By 2018, the top 10 generic drug makers controlled 70% of the market. Today, the top five control over half. That’s not competition-it’s consolidation. And it’s why 78% of all generic price spikes over 100% happen in markets with three or fewer manufacturers, according to Harvard Medical School research.
Year-by-Year Price Trends You Can’t Ignore
On paper, generic drug prices have been falling overall. But that’s an average. The real story is hidden in the outliers. Between January 2022 and January 2023, about 40 generic drugs saw price increases averaging 39%. One of them? Lisinopril, a common blood pressure pill. GoodRx data shows its cash price at Walmart jumped 247% in that same period-from $4 to $45. That’s not inflation. That’s market failure. Meanwhile, the overall list price of generics only rose 4.9% in 2023, down from 5.2% in 2022. That sounds good-until you realize it’s masking dozens of drugs that cost double or triple what they did just a year before. The FDA says 60% of generics stay stable. But the other 40%? That’s where the pain lives.Why Prices Jump Even When Nothing Changes
You’d think if a drug has been around for 10 years, its price would settle. But that’s not how it works. Manufacturers don’t set prices based on cost. They set them based on what they think they can get away with. If a drug has only one or two makers, and patients have no alternatives, the manufacturer can raise prices without losing customers. And they do. Supply chain problems make it worse. In 2023, the FDA found quality issues in 23% of foreign generic drug factories. When one factory gets shut down for not meeting standards, production drops. Prices spike. Sometimes, the shortage lasts six months or more. And during that time, the few remaining makers raise prices to cover lost volume. Even pharmacy reimbursement systems add to the chaos. Pharmacies get paid based on something called Average Wholesale Price (AWP)-a number that often has nothing to do with what they actually paid for the drug. The gap between what pharmacies pay and what they get reimbursed? On average, 22%. For small pharmacies, that’s a death sentence when a generic’s price suddenly doubles.Who Gets Hurt the Most
It’s not just patients. Pharmacists, insurers, and even Medicare are feeling the squeeze. In 2024, 37% of Medicare beneficiaries taking generics said they skipped doses or cut pills in half because of cost. Nearly 3 in 10 said they went without medication entirely. These aren’t rare stories. They’re routine. Independent pharmacies report that 42% of them had to absorb price hikes on 15% of their generic inventory. One day, a drug is profitable. The next, it’s a loss leader. Many can’t afford to keep stocking it. Patients then get told, “We don’t carry that anymore,” and have to go elsewhere. And here’s the irony: the people who save the most money on generics are the ones using discount tools like GoodRx. Their average savings? $112.50 per prescription. But if you’re on Medicaid, Medicare, or just paying cash without a coupon, you’re at the mercy of the market.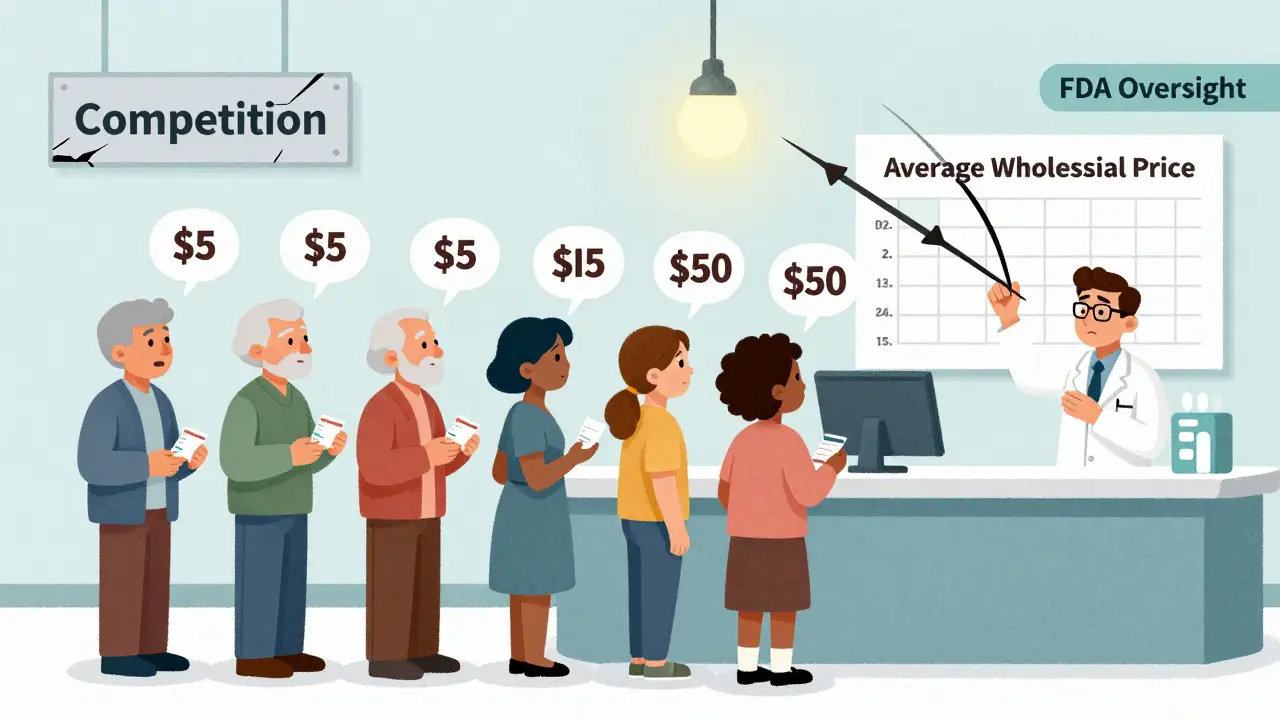
What’s Being Done-and What’s Not
The government knows this is a problem. The FTC has 12 active investigations into unjustified generic drug price hikes. The FDA is trying to speed up approvals for generics made by fewer than three manufacturers. The Inflation Reduction Act removed a cap on Medicaid rebates, which led to some brand-name price drops in early 2024-but generics barely budged. The real fix? More competition. More manufacturers. Less consolidation. But that’s easier said than done. Building a drug factory costs tens of millions. Regulatory hurdles are high. And if you’re a manufacturer, why risk investing in a drug that could crash in price overnight if someone else enters the market?What You Can Do Right Now
You can’t control the market. But you can control how you pay.- Use GoodRx, SingleCare, or RxSaver before you pay at the pharmacy. Prices vary wildly between stores-even within the same chain.
- Ask your doctor about therapeutic alternatives. Sometimes another generic in the same class is cheaper.
- Switch to a 90-day supply if your plan allows it. Bulk discounts often kick in.
- Call your pharmacy and ask if they have a cash price. Sometimes it’s lower than your insurance co-pay.
- Report sudden price spikes to your state’s attorney general. Consumer complaints trigger investigations.
The Bottom Line
Generic drugs are still the best way to save on prescriptions. But they’re no longer the predictable, low-cost option they used to be. Prices are no longer tied to production cost or competition. They’re tied to market power-and when power is concentrated, prices rise. The system isn’t broken. It’s working exactly as designed-for the companies that control it. For everyone else? It’s a gamble. One that’s getting riskier every year.Why do generic drug prices go up when no one else is making the drug?
When only one or two companies make a generic drug, there’s no competition to push prices down. These manufacturers can raise prices because patients have no other choice. This often happens after a competitor shuts down, gets acquired, or stops production due to quality issues or low profit margins. The FDA has documented cases where prices jumped over 1,000% after just one manufacturer left the market.
Are generic drugs always cheaper than brand-name drugs?
Most of the time, yes. Generic drugs typically cost 80-85% less than their brand-name equivalents. But there are exceptions. Some generics, especially those with limited competition, can cost more than the original brand-especially after a price spike. In rare cases, a generic may be priced higher because the brand-name version was already discounted through rebates or coupons.
How can I find the lowest price for my generic medication?
Use price comparison tools like GoodRx, SingleCare, or RxSaver. These sites show cash prices at local pharmacies and often have coupons that beat insurance co-pays. Prices can vary by hundreds of dollars between nearby pharmacies-even within the same chain. Always ask the pharmacist for the cash price before you pay. Sometimes it’s lower than your insurance rate.
Why do some generic drugs disappear from pharmacy shelves?
Many generic drugs are made in foreign factories. If the FDA finds quality issues-like contamination or poor manufacturing standards-it can shut down production. This causes shortages. If only one manufacturer makes the drug, and they stop producing it, pharmacies can’t restock. That’s when prices spike or the drug vanishes entirely. The FDA says 35% of generic shortages are linked to price increases over 50%.
Is there a way to avoid being hit by a sudden generic drug price increase?
Yes. Stay informed. Check your prescription prices every few months using a price-comparison app. Talk to your pharmacist about alternatives-sometimes a different generic brand or even a similar drug in the same class is cheaper. If you’re on Medicare or Medicaid, ask about prior authorization or step therapy programs that might cover a lower-cost option. And if you see a price jump of more than 20% in a month, report it to your state’s attorney general’s office.


Tony Du bled
December 21, 2025 AT 13:36Been there. Got the bill. $45 for lisinopril? That’s not healthcare, that’s extortion. And they wonder why people skip doses.
Cara Hritz
December 22, 2025 AT 11:05so like… why dont we just make more generics?? like its not rocket science?? why is this even a problem??
Johnnie R. Bailey
December 23, 2025 AT 15:44It’s not about supply-it’s about control. The pharmaceutical industry didn’t just stumble into this oligopoly. It was engineered. Consolidation isn’t accidental; it’s the result of decades of deregulation, lobbying, and the quiet dismantling of antitrust enforcement. When you have five companies controlling half the market, they’re not competing-they’re colluding, tacitly or otherwise. The FDA can approve generics all day, but if the manufacturing infrastructure is concentrated in a handful of overseas plants with zero redundancy, you’re one FDA shutdown away from a nationwide price spike. This isn’t capitalism. It’s feudalism with pill bottles.
Sam Black
December 24, 2025 AT 23:04My aunt in Sydney pays $8 AUD for the same lisinopril. She doesn’t need GoodRx. She just walks into a pharmacy. The U.S. system is a joke. We don’t have a healthcare system-we have a profit-maximization simulator.
Kathryn Weymouth
December 25, 2025 AT 15:17I work in a community pharmacy. We’ve had to stop stocking three generics in the last six months because the price jumped 200% and insurance reimbursement didn’t budge. We lose money every time we dispense them. Patients don’t understand why we can’t just order more. We’re not hoarding-we’re going bankrupt trying to keep them stocked.
Kiranjit Kaur
December 26, 2025 AT 16:48Just checked GoodRx-my metformin went from $10 to $42 in 3 months. I’m not even mad. I’m just… exhausted. 😔
Art Van Gelder
December 27, 2025 AT 17:05Think about this: the same company that makes your generic blood pressure pill also owns the factory in India that produces the active ingredient. That same company also owns the distributor that sells to your local pharmacy. That same company also lobbied Congress to block the FDA from requiring transparency on pricing. So when the price jumps from $4 to $45, it’s not a market fluctuation-it’s a corporate algorithm. And you’re the variable they’re optimizing. We’ve turned medicine into a derivatives trading floor, and the only thing that matters is the spread between what it costs to make and what they can charge before the next audit. It’s not capitalism. It’s a rigged casino with a stethoscope.
Jim Brown
December 28, 2025 AT 17:56There is a profound moral inversion at work here. We have commodified the very substances that sustain life, and then we have constructed a system wherein access to those substances is contingent upon the ability to navigate a labyrinth of pricing opacity, corporate consolidation, and regulatory capture. The notion that competition naturally lowers prices assumes the existence of competition. But when markets are hollowed out by strategic acquisition, when innovation is stifled by the threat of price erosion, and when the state abdicates its responsibility to ensure equitable access, we are no longer in a market-we are in a managed scarcity. The generic drug crisis is not an economic anomaly. It is the logical endpoint of neoliberal governance applied to human biology.
Aliyu Sani
December 30, 2025 AT 09:59bro the whole system is just a pyramid scheme. big pharma owns the patents, then sells the rights to a shell corp, then that corp owns 3 factories in china, then they shut one down cause its cheaper to raise prices than to fix the machine. its not even a game anymore. its just a machine that grinds people down. and we just sit here and pay.
Gabriella da Silva Mendes
December 30, 2025 AT 14:55USA. 🇺🇸. We do everything better. Except healthcare. And generics. And pricing. And regulation. And… wait, actually we’re just terrible at everything that involves human care. 💀
Nader Bsyouni
January 1, 2026 AT 02:07you people act like this is new. since when did we expect capitalism to care about your thyroid
Tarun Sharma
January 1, 2026 AT 11:53Price spikes occur due to market concentration. Regulatory inefficiencies exacerbate supply chain fragility. Policy intervention must focus on incentivizing diversification of manufacturing and enforcing antitrust measures.
Jamison Kissh
January 2, 2026 AT 06:22What if the real problem isn’t the price of the drug-but the fact that we’ve outsourced the entire production chain to countries with zero transparency, no labor protections, and no accountability? We don’t just import pills-we import risk. And when a factory in Telangana gets shut down for unsanitary conditions, suddenly your blood pressure med becomes a luxury item. We treat medicine like a commodity, but we forget it’s a biological necessity. The system doesn’t fail because it’s broken-it fails because it was never designed to protect people.
Sai Keerthan Reddy Proddatoori
January 3, 2026 AT 20:45India makes 80% of the world's generics. But our government gives them to poor people for free. America lets corporations steal from sick people. This is why we are better. You need to stop begging for coupons and fix your system.
Julie Chavassieux
January 4, 2026 AT 16:30…