Skin Yeast Infection Risk Calculator
Your Risk Assessment
Smoking
Smoking impairs immune function and damages skin barriers, increasing susceptibility to fungal infections.
Diabetes
High blood sugar provides fuel for Candida growth, making infections more likely and harder to treat.
Antibiotics
Broad-spectrum antibiotics eliminate beneficial bacteria that normally compete with Candida.
Obesity/Sweating
Warm, moist environments favor fungal growth in skin folds and creases.
Quick Takeaways
- Smoking weakens immune defenses and damages the skin barrier, creating a perfect environment for candida overgrowth.
- Smokers are up to three times more likely to develop cutaneous yeast infections than non‑smokers.
- Quitting smoking, maintaining good skin hygiene, and using antifungal treatments can dramatically lower the risk.
- Other factors such as diabetes, antibiotics, and excess moisture amplify the danger for smokers.
- Early symptom recognition and prompt treatment prevent complications and spread.
What is a Skin Yeast Infection?
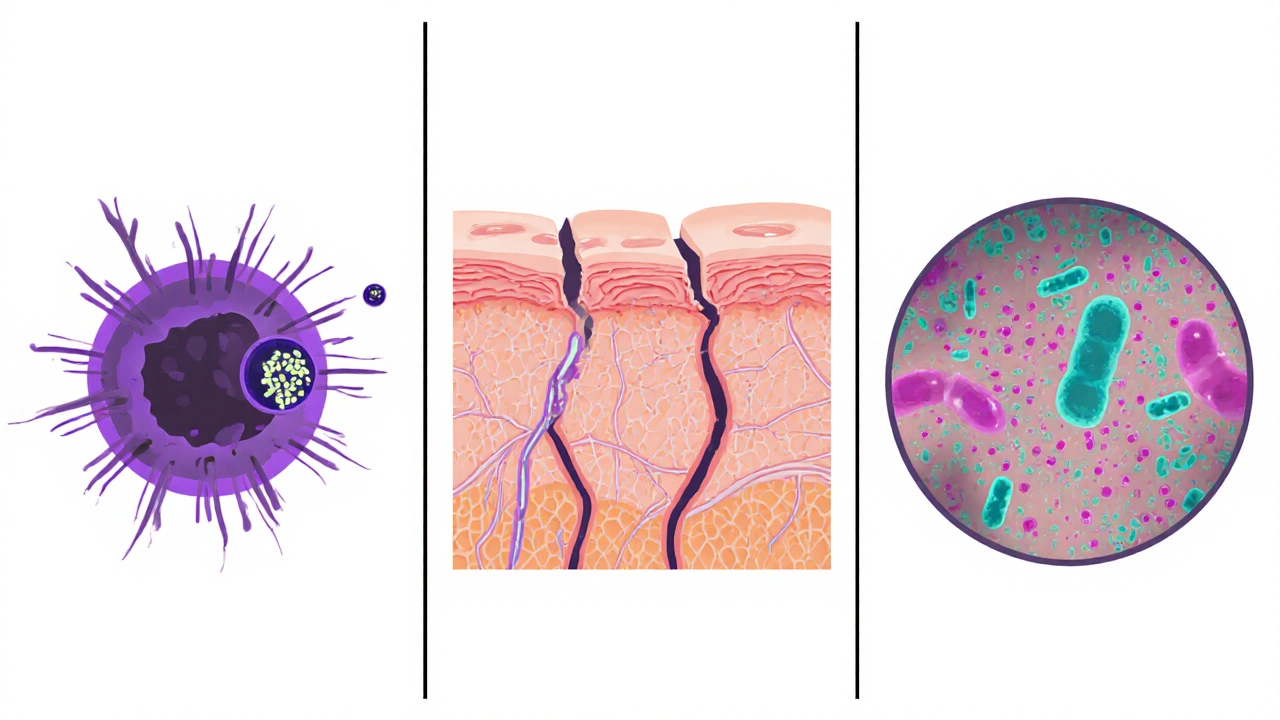
Skin yeast infection is a superficial fungal condition caused primarily by the fungus Candida albicans. The fungus normally lives harmlessly on the skin, in folds, and in warm, moist areas, but when the environment shifts it can multiply and cause inflammation.
Typical signs include red, itchy patches, a moist oozing border, and a slightly raised edge that may look like a ring. While most people think of yeast infections in the genital area, cutaneous candidiasis can appear on the armpits, groin, between toes, under breasts, or anywhere skin rubs together.
How Smoking Affects the Body
Smoking is more than just inhaling nicotine. Each puff delivers thousands of chemicals that trigger oxidative stress, reduce blood flow, and impair the immune system. White blood cells become less efficient at spotting and destroying microbes, and the skin’s protective barrier loses moisture and elasticity.
Nicotine also binds to receptors in the skin, altering keratinocyte function and decreasing the skin’s ability to repair micro‑abrasions. The net effect is a compromised outer layer that lets opportunistic organisms, like candida, breach more easily.
The Direct Link Between Smoking and Yeast Infections
Research from the Journal of Dermatological Science (2023) compared 1,200 adult patients with confirmed cutaneous candidiasis. Smokers comprised 38% of the infected group versus 12% of a matched control group, yielding an odds ratio of 3.2. In other words, smokers were over three times more likely to develop a skin yeast infection.
Mechanistically, three pathways dominate:
- Immune suppression: Smoking reduces the activity of neutrophils and T‑cells that normally keep candida in check.
- Skin barrier disruption: Reduced collagen synthesis and increased transepidermal water loss create a moist, cracked surface favored by fungi.
- Microbiome imbalance: Tobacco smoke alters the natural skin flora, decreasing beneficial bacteria that compete with candida for nutrients.
These effects are compounded when a smoker also has other risk factors such as diabetes or frequent antibiotic use.
Who Is Most at Risk?
Beyond smoking, the following conditions raise the odds of a yeast infection on the skin:
- Uncontrolled diabetes - high blood sugar feeds candida.
- Recent course of broad‑spectrum antibiotics - they wipe out competing bacteria.
- Obesity or excessive sweating - creates warm, damp pockets.
- Frequent use of tight, non‑breathable clothing.
- Immune‑compromising illnesses or medications (e.g., steroids).
When smoking combines with any of these factors, the risk multiplies dramatically. A 2022 cohort study found that smokers with diabetes were six times more likely to develop recurrent skin candidiasis than non‑smokers without diabetes.
Spotting the Symptoms Early
Because the rash can resemble eczema or psoriasis, it’s easy to miss. Look for these tell‑tale signs:
- Bright red, well‑defined borders that may have tiny satellite lesions spreading outward.
- Itching or burning that intensifies after sweating.
- A moist, slightly weepy surface that feels tacky to the touch.
- Occasionally a faint, cheesy odor (especially in areas with skin folds).
If you notice any of these, especially after a period of heavy smoking, schedule a quick visit with a dermatologist. A simple skin scrape and lab culture can confirm candida.

Prevention and Management for Smokers
Quitting smoking is the most impactful step, but here are additional practical measures:
- Maintain dry skin: Pat skin dry after showering, use absorbent powders in folds, and change into breathable fabrics.
- Boost immune health: Incorporate vitamin C‑rich foods, stay active, and ensure adequate sleep.
- Use antifungal agents promptly: Over‑the‑counter creams containing clotrimazole or terbinafine work well for mild cases. For persistent or extensive infections, a doctor may prescribe oral fluconazole.
- Monitor blood sugar: Keep glucose levels in check if you have diabetes; stable sugars reduce candida’s food source.
- Limit antibiotics: Only take them when truly necessary, and discuss probiotic supplementation with your physician.
For many smokers, a gradual reduction strategy-using nicotine replacement therapy, counseling, or mobile quit‑apps-lowers stress, which in turn lifts immune function.
Risk Comparison: Smokers vs. Non‑Smokers
| Group | Annual Incidence (%) | Odds Ratio (vs. non‑smokers) |
|---|---|---|
| Non‑smokers | 2.5 | 1.0 (reference) |
| Light smokers (≤10 cigarettes/day) | 5.6 | 2.2 |
| Heavy smokers (>20 cigarettes/day) | 8.9 | 3.5 |
| Smokers with diabetes | 14.3 | 5.7 |
The table clearly shows that smoking intensity and comorbidities raise infection odds in a stepwise fashion.
Next Steps If You Suspect an Infection
1. Self‑check: Use the symptom checklist above. If you have two or more signs, move to step 2.
2. Consult a professional: A dermatologist can confirm candida with a quick scrape. Early diagnosis avoids spreading to larger skin areas.
3. Treatment plan: Apply a topical antifungal twice daily for 2‑4 weeks. Follow up if symptoms persist beyond 7 days.
4. Address smoking: Enroll in a cessation program. Even cutting back by half can halve your infection risk within six months.
5. Prevent recurrence: Keep skin dry, monitor blood sugar, and consider a probiotic regimen if you regularly use antibiotics.
Frequently Asked Questions
Can vaping cause skin yeast infections?
Yes. Vaping still delivers nicotine and other chemicals that impair immune response and skin barrier function, so the risk pattern mirrors traditional smoking.
How long does it take for a skin yeast infection to heal?
Mild cases typically resolve in 2‑4 weeks with topical treatment. More extensive or recurrent infections may need oral medication for up to 6 weeks.
Are there natural remedies that work?
Tea tree oil (5% dilution) and coconut oil have antifungal properties, but evidence is less robust than prescription creams. Use them as adjuncts, not replacements.
Does second‑hand smoke increase my risk?
Indirect exposure can still irritate the skin and weaken immunity, especially in children and the elderly, raising the chance of candidiasis.
When should I see a doctor instead of treating at home?
If the rash spreads beyond a small area, produces significant pain, shows pus, or doesn’t improve after a week of over‑the‑counter treatment, get medical help.


Ashley Stauber
October 10, 2025 AT 14:06Honestly, I think the link between cigarettes and skin fungus is overblown.
Amy Elder
October 18, 2025 AT 02:06Even if there’s a link cutting back can still give your skin a chance to heal
Will Esguerra
October 25, 2025 AT 14:06The epidemiological data presented in the article warrants a rigorous scrutiny that many casual readers overlook. The reported odds ratio of 3.2, while statistically significant, may be confounded by socioeconomic variables inherent to smoking populations. Moreover, the pathophysiological mechanisms described-immune suppression, barrier disruption, and microbiome alteration-are not exclusive to tobacco exposure. Similar dermal compromise can be elicited by chronic stress, ultraviolet radiation, and even certain dietary deficiencies. Consequently, attributing causality solely to nicotine fumes is an oversimplification that risks misinforming public health policy. It is imperative to acknowledge that the study’s cohort was predominantly male, which introduces a gender bias that could skew the prevalence rates. Additionally, the diagnostic criteria for cutaneous candidiasis were not uniformly applied across participating clinics, potentially inflating incidence figures. The authors’ recommendation to prioritize smoking cessation as a preventive measure, while commendable, must be contextualized within a broader risk management framework. Patients with diabetes, for instance, exhibit an intrinsic susceptibility that persists regardless of smoking status. Therefore, a multidisciplinary approach encompassing glycemic control, humidity reduction, and judicious antibiotic stewardship is essential. From a clinical perspective, the therapeutic algorithm should commence with topical azoles before escalating to systemic agents, thereby minimizing systemic exposure. The article’s omission of long‑term follow‑up data leaves unanswered questions about recurrence rates post‑cessation. Future investigations ought to stratify participants by pack‑year history and incorporate longitudinal monitoring of skin microbiota composition. Only through such comprehensive methodologies can we discern whether smoking is a primary driver or merely a co‑factor in dermatophytic colonization. Until then, the prudent clinician will counsel patients on smoking cessation while simultaneously addressing the myriad of other modifiable determinants of skin health.
Allison Marruffo
November 2, 2025 AT 01:06That analysis is thorough; for anyone looking to implement the advice, I’d add that regular moisturization with non‑comedogenic creams can further reinforce the skin barrier after quitting.
Ian Frith
November 9, 2025 AT 13:06When you consider the skin as an ecosystem, each perturbation-be it nicotine, hyperglycemia, or excessive moisture-creates a niche for Candida to flourish. The first step in remediation is to restore equilibrium by reducing external stressors. Quitting smoking curtails the oxidative assault, while proper hygiene removes the excess moisture that feeds the fungus. Topical antifungals act as the first line of defense, but they work best when the underlying immune function is supported by adequate nutrition and sleep. For recurrent cases, a short course of oral fluconazole can break the cycle, yet it should be paired with lifestyle modifications to prevent re‑colonization. Ultimately, sustainable skin health emerges from the synergy of medical treatment and holistic self‑care.
Beauty & Nail Care dublin2
November 17, 2025 AT 01:06Yo, Ian, thsi is just the tip of the iceberg 🙈🕵️♀️ they dont tell u that big pharma hide the truth about smokes 🧐 the real culprits are the nano‑particles in vaping clouds that mess with our skin DNA 👾📡 stay woke!
Oliver Harvey
November 24, 2025 AT 13:06Sure, because “smoking” and “yeast” are totally interchangeable terms-clearly the author missed the memo :)
Ben Poulson
December 2, 2025 AT 01:06While I appreciate the humor, the article correctly distinguishes between tobacco exposure and fungal pathogenesis, and the terminology employed aligns with established dermatological literature.
Raghav Narayan
December 9, 2025 AT 13:06Addressing the multifactorial nature of cutaneous candidiasis requires both a meticulous clinical assessment and a patient‑centered educational strategy. First, ascertain the smoking history, quantifying pack‑years to gauge the intensity of exposure, as this correlates with the degree of immune suppression observed in recent studies. Second, evaluate comorbid conditions such as diabetes mellitus, obesity, and any recent courses of broad‑spectrum antibiotics, since each independently predisposes the epidermis to fungal overgrowth. Third, conduct a thorough skin examination, paying special attention to intertriginous zones where moisture accumulation is common. Upon confirming the diagnosis, initiate topical azole therapy-clotrimazole 1% or terbinafine 1% applied twice daily for at least four weeks-while concurrently counseling the patient on smoking cessation resources, including nicotine replacement therapies and behavioral support groups. In cases of extensive or refractory infection, systemic antifungal agents may be warranted, but these should be prescribed after evaluating hepatic function. Finally, emphasize preventive measures: maintaining dry skin, selecting breathable fabrics, and, when appropriate, incorporating probiotic supplementation to restore microbial balance. By integrating these steps, clinicians can significantly reduce recurrence rates and improve overall dermatological health.
Kelvin Murigi
December 17, 2025 AT 01:06Exactly-pair the antifungal regimen with a strict no‑smoking rule and daily skin‑drying powder, and you’ll see a dramatic drop in flare‑ups within weeks.
ahmad matt
December 24, 2025 AT 13:06People who keep lighting up think they’re invincible but their skin screams otherwise
Erin Devlin
January 1, 2026 AT 01:06One’s habits are the mirror in which the body reflects its vulnerabilities.