When you pick up a prescription, you might be handed a pill bottle with a different name than what your doctor wrote on the script. That’s not a mistake-it’s pharmacy substitution. In most states, pharmacists are allowed to swap a brand-name drug for a cheaper generic version, unless your doctor says otherwise. But here’s the catch: the rules aren’t the same everywhere. What’s legal in Texas might be blocked in Hawaii. And if you’re switching to a biosimilar for a biologic drug like Humira or Enbrel, the rules get even more complicated.
What Exactly Is Pharmacy Substitution?
Pharmacy substitution means a pharmacist replaces the brand-name drug your doctor prescribed with a generic version that’s chemically identical. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration as the brand. They must also work the same way in your body. That’s why most people can safely switch without issues. But not all drugs are created equal. For medications with a narrow therapeutic index-like warfarin, lithium, or phenytoin-even tiny differences in how the body absorbs the drug can cause serious side effects. That’s why some states ban substitution for these drugs entirely. And then there are biosimilars. These aren’t generics. They’re copies of complex biologic drugs made from living cells. The FDA has a special label for them: “interchangeable.” Only 10 out of 38 approved biosimilars have that label as of late 2023. Even then, states can still block substitution unless the pharmacist follows strict rules.How Your State Rules Work
All 50 states and Washington, D.C. have laws about substitution, but they fall into three main categories. Permissive states (31 + DC): Pharmacists can substitute, but they don’t have to. They’ll usually do it unless the doctor says “do not substitute” or you refuse. This is the most common model. Mandatory states (19): Pharmacists must substitute unless the prescription says “dispense as written.” These states assume generics are just as safe and want to cut costs wherever possible. Restrictive states (none officially, but some act like it): Some states have lists of drugs that can’t be swapped-like antiepileptics in Hawaii or certain biologics in Kentucky. Others require extra steps, like getting your doctor’s permission before switching.Do You Need to Give Consent?
This is where things get messy. In 7 states and D.C., pharmacists need your explicit consent before swapping a drug. That means they have to ask you, “Do you want this generic instead?” and you say yes. In 31 states and D.C., they only need to notify you after the fact. You might get a printed notice or hear it from the pharmacist, but you don’t get a chance to say no beforehand. And in 19 states, there’s no requirement to tell you at all. You just get the generic, and you might not know until you check the label or get a bill. The problem? You have the right to refuse substitution in every state. But if no one tells you that, you can’t exercise it.What About Biosimilars?
Biosimilars are trickier. They’re not like simple generics. Because they’re made from living cells, even small changes in the manufacturing process can affect how they work. The FDA says they’re “highly similar” to the original, but not identical. Only drugs labeled “interchangeable” can be swapped automatically. As of late 2023, only 10 biosimilars have that status. Even then, 45 states have extra rules for them. In 37 states, the pharmacist must notify your doctor within a few days after swapping. In 12 states, they need your doctor’s permission before switching. And in 15 states, they can’t substitute if the biosimilar costs more than the original-even if your insurance covers the cheaper one. States like Florida and Illinois require both patient and prescriber notification within 24-72 hours. Alabama and Mississippi? Just document it and move on.
What Can You Do as a Patient?
You don’t have to sit back and wait for the pharmacist to decide for you. Here’s what works:- Ask upfront. When you hand over your prescription, say: “Can this be substituted for a generic?”
- Check the label. The drug name on the bottle should match what your doctor wrote. If it doesn’t, ask why.
- Refuse if you want. You can say no to substitution at any time, even if you’ve already taken the generic. Pharmacists can’t force you.
- Get your doctor to write “dispense as written.” If you’ve had bad reactions to generics before, or you’re on a narrow therapeutic index drug, ask your doctor to add this note to your prescription.
- Know your state’s rules. Visit your state board of pharmacy website. Most have a page listing substitution laws. If you can’t find it, call them. They’re required to answer.
What Pharmacists Must Do
Pharmacists aren’t free to substitute however they want. They have to:- Check if the drug is on any state-specific substitution lists.
- Verify the prescription doesn’t say “dispense as written.”
- Confirm the generic is FDA-approved and pharmaceutically equivalent.
- Document the substitution in your record-most states require this for at least two years.
- Notify you if required by law (and in many cases, even if not required, they do it anyway).
Why This Matters for Your Health
The goal of substitution laws is simple: save money. Generic drugs cost 80-85% less than brand names. In 2023, generics saved the U.S. healthcare system $313 billion. That’s real money-money that keeps prescriptions affordable for millions. But savings shouldn’t come at the cost of safety. A 2018 study found that states with restrictions on substituting narrow therapeutic index drugs had 18% fewer adverse events. That’s why some drugs-like seizure meds, blood thinners, and thyroid hormones-are protected in certain states. The bigger issue? Confusion. A 2022 survey found 67% of pharmacists initially didn’t understand the difference between “biosimilar” and “interchangeable.” If they’re unsure, you might get the wrong drug-or miss out on a cheaper option.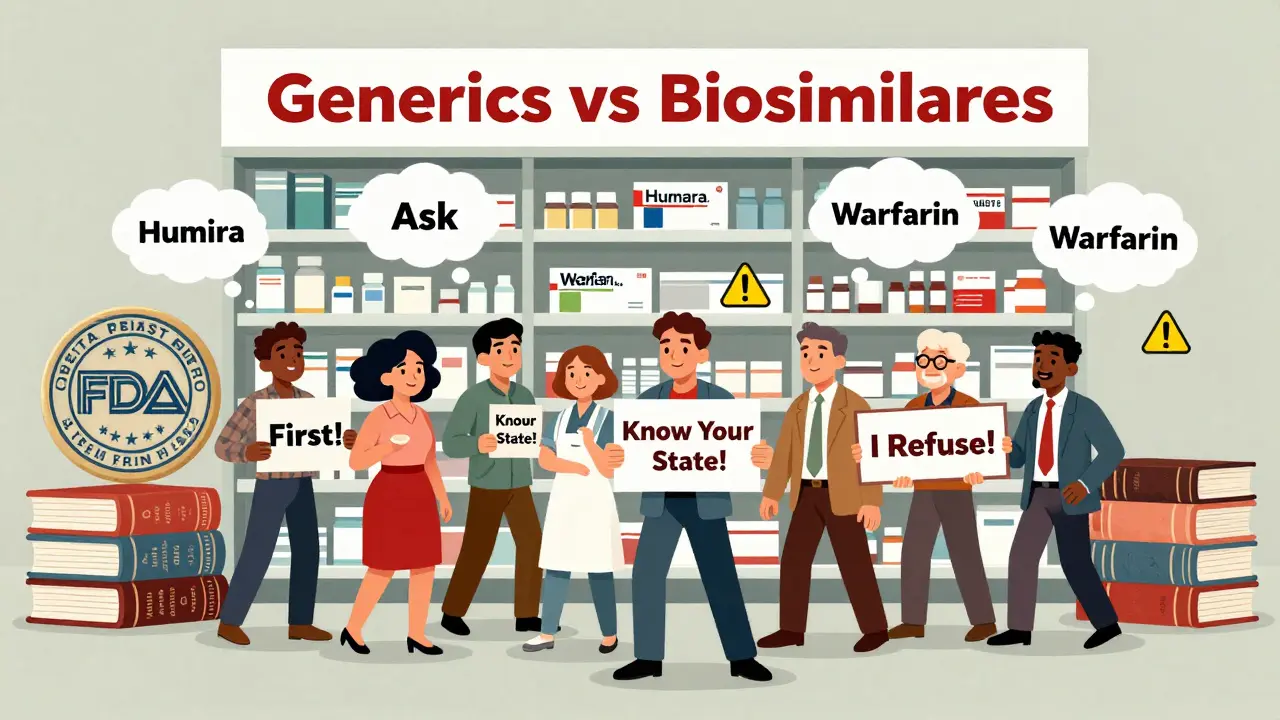
How to Find Your State’s Rules
You don’t need to be a lawyer to understand your rights. Here’s how to find your state’s substitution laws:- Go to your state board of pharmacy website. Search “[Your State] board of pharmacy substitution laws.”
- Look for “Drug Product Selection” or “Generic Substitution” sections.
- Check if your state is mandatory, permissive, or has a negative formulary (list of non-substitutable drugs).
- See if there are special rules for biologics or biosimilars.
- Call the board if you can’t find it online. They’re required to help.
What’s Changing in 2026?
More biosimilars are getting “interchangeable” status. That means more drugs will be eligible for automatic substitution. California and New York updated their laws in early 2023 to require clearer patient notifications. Other states are following. Expect more states to adopt consistent documentation rules and notification timelines. The goal? Reduce confusion for patients and pharmacists alike. But until then, you’re the best advocate for your own care. Don’t assume the pharmacist knows your history. Don’t assume the generic is always the right choice. And don’t be afraid to ask questions.Frequently Asked Questions
Can my pharmacist substitute my brand-name drug without telling me?
In 19 states, yes-they’re not required to notify you. In 31 states and D.C., they must notify you after substitution. Only 7 states and D.C. require your consent before switching. Always check your prescription label and ask if you’re unsure.
What if I don’t want a generic drug?
You can refuse substitution at any time, no matter what your state’s law says. Just tell the pharmacist, “I don’t want this generic.” They must fill the prescription as written. If they refuse, contact your state board of pharmacy.
Are biosimilars safe to switch to?
Only biosimilars labeled “interchangeable” by the FDA are approved for automatic substitution. As of late 2023, only 10 out of 38 approved biosimilars have that status. Even then, your state may require your doctor to be notified or give permission. Always confirm with your pharmacist whether the biosimilar you’re being offered is interchangeable.
Why does my doctor write “dispense as written” on my prescription?
It means they don’t want the pharmacy to substitute a generic. This is common for drugs with narrow therapeutic indexes, like warfarin or seizure medications. In 18 states, the doctor must explain why they’re blocking substitution. In others, they don’t have to. Either way, the pharmacist must follow it.
Do I have to pay more if I refuse a generic?
Sometimes. Insurance plans often have lower copays for generics. If you refuse substitution, you may pay the full brand-name price unless your plan has an exception. Ask your pharmacist or insurer about your out-of-pocket cost before refusing.


jefferson fernandes
January 14, 2026 AT 13:27Look, I get that generics save money-but I’ve had seizures from a generic version of my epilepsy med, and now I refuse them outright. My doctor writes ‘dispense as written’ on every script. If your state doesn’t require consent, that’s a dang safety hazard. Pharmacists aren’t doctors-they shouldn’t be playing Russian roulette with your brain.
And don’t even get me started on biosimilars-those aren’t generics! They’re like a photocopy of a photocopy of a Picasso. Some of them work fine, but others? You feel like your body’s been hijacked by a robot. I’ve had three different biosimilars for my RA-each one felt different. The pharmacy didn’t even tell me I was switched until I noticed the bottle looked wrong.
States need to mandate pre-substitution consent. Period. Full stop. If you’re going to swap a drug that could kill you, you damn well better ask first.
Also-why are we letting pharmacists decide what’s ‘safe’? That’s a medical decision. Not a cost-cutting one. I’m tired of being treated like a spreadsheet cell.
Milla Masliy
January 14, 2026 AT 15:24As someone who grew up in a family that couldn’t afford brand-name meds, I’m all for generics. But I’ve seen my mom panic because she didn’t know she’d been switched to a different version of her thyroid med-she thought she was having a heart attack, but it was just the filler changing how it absorbed.
Maybe we need a universal ‘substitution alert’ sticker on every prescription bottle? Like, a little yellow flag that says: ‘This is NOT what your doctor prescribed. You have a right to refuse.’
And for biosimilars? Yeah, they’re expensive to make, but if they’re labeled ‘interchangeable,’ why are states still blocking them? Sounds like pharmacy bureaucracy running wild. Let’s simplify, not complicate.
sam abas
January 15, 2026 AT 04:15Okay so let me get this straight-some states say you can swap, some say you can’t, some say you have to ask, some say you have to tell, some say biosimilars are fine unless they cost more than the original-which is literally the opposite of economic logic-and nobody can agree on whether a pharmacist can just hand you a pill bottle and say ‘here’s your medicine’ without telling you it’s not what your doctor ordered?
And yet we’re surprised people don’t trust the healthcare system?
Also, ‘interchangeable’ is a marketing term, not a medical one. The FDA doesn’t test for ‘equivalence in real life,’ they test for ‘equivalence in a lab under controlled conditions.’ That’s like saying two cars are interchangeable because they both have four wheels and an engine. One’s a Prius, one’s a tank.
And why is nobody talking about how insurance companies force these switches? Pharmacists are just the middlemen. The real villains are the PBMs who get kickbacks from generic manufacturers.
Also, typo: ‘dispense as written’ is not a legal term, it’s a prescription instruction. Don’t quote me on that though, I’m just a guy on the internet with too much time and a pharmacy degree I never finished.
John Pope
January 16, 2026 AT 10:05Let’s be real here-this isn’t about patient safety. It’s about power. Who gets to decide what goes into your body? The doctor? The pharmacist? The insurance company? The state legislature? The pharmaceutical conglomerate that owns the patent on the brand and the generic?
It’s all a theater. You think your ‘right to refuse’ means anything when you’re handed a bottle and told ‘this is your medication’? You’re not a patient-you’re a consumer. And consumers don’t get to negotiate terms. They get to pay.
And biosimilars? Oh, please. They’re not ‘highly similar.’ They’re ‘close enough for government work.’ That’s the official FDA definition, by the way. I’m not making this up. You’re being sold a placebo with a fancy name and a 70% discount.
And yet, we’re told to trust the system. Trust the label. Trust the pharmacist. Trust the state. Trust the invisible hand of the market.
Meanwhile, your grandma’s blood pressure spikes because she was switched to a generic warfarin and nobody told her. Again.
Wake up. This isn’t healthcare. It’s corporate choreography with a stethoscope.
vishnu priyanka
January 18, 2026 AT 04:12Man, I came from India where generics are the only thing people can afford-and we still call them ‘branded generics’ because the name matters. Here in the US, you treat generics like they’re some kind of shame. But in Delhi, if your kid’s asthma inhaler costs $2 instead of $200, you don’t ask questions-you just take it.
Still, I get the fear. My cousin got sick after switching to a generic anticonvulsant. Turned out the filler had a weird reaction with his liver enzymes. Nobody warned him.
So yeah-maybe the system’s broken. But the solution isn’t to ban substitution. It’s to make the labeling clearer. Add a QR code to the bottle that links to a simple video: ‘This is not your original drug. Here’s why it’s safe. Here’s when to call your doctor.’
Simple. Human. No bureaucracy. Just info.
Angel Molano
January 19, 2026 AT 20:56You people are panicking over nothing. Generics are safe. If you can’t handle a $5 pill instead of a $50 one, you shouldn’t be on meds. Stop being dramatic. The system works. You just don’t like it because you’re lazy.
Vinaypriy Wane
January 21, 2026 AT 19:35I’ve been a pharmacist for 18 years, and I’ve seen what happens when patients don’t know they’ve been switched. One woman came in crying because she thought her antidepressant stopped working-turns out, the generic had a different coating, and it wasn’t dissolving fast enough. She didn’t know she could say no.
So I started asking every patient: ‘Hey, do you want the generic?’ Even if the law doesn’t require it. Because it’s the right thing to do.
And yes, I’ve lost sales because of it. But I sleep better at night.
Also, biosimilars? I’ve had patients report mood swings, fatigue, even rashes after switching. We don’t have long-term data. We’re guessing. And that’s not okay.
Just ask. It takes 10 seconds. And if they say no? You respect it. That’s what medicine is supposed to be.
Randall Little
January 23, 2026 AT 11:35So let me get this straight: in 19 states, you can legally be handed a different drug without being told? And we call this ‘healthcare’?
Meanwhile, in 7 states, you have to give consent. So… we’re just now realizing that people should have a say in what enters their body?
That’s not a policy failure. That’s a moral failure dressed up as a regulatory gray area.
And the fact that ‘interchangeable’ biosimilars are still rare? That’s not science. That’s corporate lobbying. The same companies that made the original biologics own the biosimilars. Why would they rush interchangeable status if it means they lose monopoly pricing?
Oh, and the 2022 survey said 67% of pharmacists didn’t understand the difference? That’s not incompetence. That’s systemic neglect.
So we’re trusting a profession that doesn’t even understand the drugs they’re handing out… to make life-or-death decisions… without consent?
What a country.
lucy cooke
January 24, 2026 AT 03:23Oh, darling, it’s all so terribly tragic, isn’t it? The great American pharmaceutical farce-where your body becomes a cost center and your dignity a footnote on a form. We’ve turned healing into a spreadsheet, and now we’re surprised when people feel like lab rats?
And biosimilars? How quaint. A ‘copy’ of a living molecule? As if biology could ever be replicated by a corporate R&D team in a sterile lab with a budget cut by 30%. It’s like asking a Picasso to paint a copy of himself… and then selling it as the original.
But of course, we must save money. Mustn’t we? Even if it means your immune system starts hating you for no discernible reason.
At least in London, we have a National Health Service that actually cares about outcomes, not quarterly earnings. But then again, you Americans prefer your tragedies with a side of insurance fine print.
Trevor Whipple
January 24, 2026 AT 20:53Bro. I got my ADHD med switched to generic and I felt like a zombie for two weeks. My doc said ‘dispense as written’ but the pharmacist didn’t care. I had to call the state board to get them to admit they broke the law. Now I take pics of every bottle. And I yell at every pharmacist. It’s exhausting. But I won’t die for a $15 copay.
Also, ‘interchangeable’ is just a fancy word for ‘we’re too lazy to test it properly.’
Lethabo Phalafala
January 25, 2026 AT 02:59I’m from South Africa-we don’t have brand-name drugs here. Everything’s generic. And guess what? People live. People thrive. We don’t have the luxury of choice, so we trust the science.
But I get it-some people are scared because they’ve been lied to by pharma ads. ‘This brand is special!’ Nope. It’s just more expensive.
Still… if you’ve had bad reactions before? Speak up. No one’s stopping you. Just say ‘no.’ It’s your body. Your rules.
And if the pharmacist acts like you’re being difficult? Tell them to call your doctor. That shuts them up every time.
Lance Nickie
January 25, 2026 AT 13:27Generic = good. Stop whining. If you can’t afford your med, you’re not supposed to be on it anyway. Get a job.
Clay .Haeber
January 25, 2026 AT 16:54Let’s be honest: this entire system is a joke. The FDA? A rubber stamp for Big Pharma. The pharmacists? Underpaid clerks doing the bidding of PBMs. The states? Bureaucratic mazes designed to confuse the vulnerable.
And yet we pretend this is ‘healthcare.’
Meanwhile, the real innovation isn’t in biosimilars-it’s in AI-driven personalized dosing, which no one’s funding because it doesn’t scale. We’re optimizing for profit, not people.
And you know what? I’m not even mad. I’m just… disappointed. Like, I used to believe in science. Now I just believe in spreadsheets.
Also, ‘dispense as written’? That’s not a legal term. It’s a plea for mercy.
jefferson fernandes
January 26, 2026 AT 07:17Wait-you’re telling me in 19 states, you can get switched without being told? That’s not healthcare. That’s medical identity theft. I’m calling my state rep tomorrow. This is a civil rights issue.