Switching from a brand-name medication to a generic can save money-but for some people, it’s not just about cost. It’s about safety, stability, and feeling in control of your health. If you’ve noticed changes after switching-like worse symptoms, new side effects, or lab results that don’t match up-you’re not alone. And you don’t have to accept the switch without a fight. Talking to your doctor about staying on your brand medication isn’t about being difficult. It’s about being informed and advocating for what works for your body.
Why Some People Need to Stay on Brand Medication
Not all medications are created equal, even when they have the same active ingredient. For drugs with a narrow therapeutic index, tiny differences in how the body absorbs the drug can make a big difference. Think of it like tuning a guitar: if the string is even slightly off, the whole sound changes. Medications like warfarin (for blood thinning), levothyroxine (for thyroid), and certain anti-seizure drugs like Keppra or Lamictal fall into this category. Studies show that switching from brand to generic versions of these drugs can lead to a 23% higher risk of seizure recurrence, or a 17% increase in emergency visits for people on warfarin due to unstable blood levels. Another real issue? Inactive ingredients. Generics use different fillers, dyes, or preservatives. For someone allergic to lactose, gluten, or a specific dye like FD&C Red No. 40, even a tiny amount in a generic pill can trigger a reaction. About 7% of patients report allergic or intolerant reactions to these non-active components. One patient I spoke to developed severe stomach cramps every time she switched to a generic version of her antidepressant-until she went back to the brand. Her symptoms vanished. That’s not "in her head." It’s chemistry.What Your Doctor Needs to Hear
Doctors aren’t against brand-name drugs. They’re often pressured by insurance companies to prescribe generics. But they’ll listen if you come prepared. Don’t say, “I just feel better on the brand.” That’s vague. Instead, say: “I had three seizures in two months after switching to the generic Keppra. I hadn’t had one in five years on the brand. My neurologist’s notes from last year show my drug levels dropped 30% after the switch.” Bring proof. That means:- Lab results showing changes in blood levels
- Medication logs with dates, symptoms, and severity (e.g., “March 12: headache, dizziness, blurred vision after taking generic”)
- Pharmacy receipts showing when you switched
- Any notes from specialists or pharmacists
- Situation: “I’m here because I had a bad reaction after switching to the generic version of my medication.”
- Background: “I’ve been on the brand for 3 years with no issues. After switching last month, I started having X, Y, Z symptoms.”
- Assessment: “I believe the generic is not working for me based on my history and lab results.”
- Recommendation: “Can we go back to the brand? Or test my drug levels again to confirm?”
Insurance Is the Bigger Hurdle
Even if your doctor agrees, your insurance might not. In Australia, private health insurers and Medicare Part D (in the U.S.) often require prior authorization for brand-name drugs when a generic exists. That means your doctor has to fill out paperwork explaining why the brand is medically necessary. Here’s what helps:- Ask your doctor to write “Dispense as Written” (DAW-1) on the prescription. This tells the pharmacy not to substitute.
- Provide your doctor with your documented history of problems with generics. They’ll use that in the appeal.
- Check your medication’s therapeutic equivalence rating in the FDA’s Orange Book (or Australia’s PBS database). If it’s rated AB1 or AB2, it’s considered interchangeable-but if it’s BX, that means it’s not recommended for substitution.
What to Do Before Your Appointment
Don’t walk in unprepared. Take 15 minutes before your visit to gather what you need:- Write down every time you switched to a generic and what happened. Include dates, symptoms, and how long they lasted.
- Check your last blood test results. Did your levels change after the switch?
- Look up your medication’s brand and generic names. Know the exact difference in inactive ingredients.
- Print out or screenshot your pharmacy’s dispensing history. Show when the switch happened.
- Bring the actual pill bottles-brand and generic side by side. Sometimes the difference in size, color, or smell is obvious.
What Your Doctor Might Say (And How to Respond)
Your doctor might say: “Generics are just as good. The FDA says so.” That’s true-but incomplete. The FDA says generics must be bioequivalent, meaning they deliver 80-125% of the active ingredient compared to the brand. That’s a 45% range. For most drugs, that’s fine. For others? Not enough. You can respond: “I understand generics are approved, but for my condition, even small changes in absorption have caused real problems. My doctor’s notes from last year show my levels dropped when I switched. I’m not asking for an expensive option-I’m asking for a stable one.” Another common response: “It’ll take too long to get prior auth.” Say: “I’m happy to help. I’ve got all my records ready. Can we start the process today?” Doctors are stretched thin. If you make it easy for them to say yes, they will.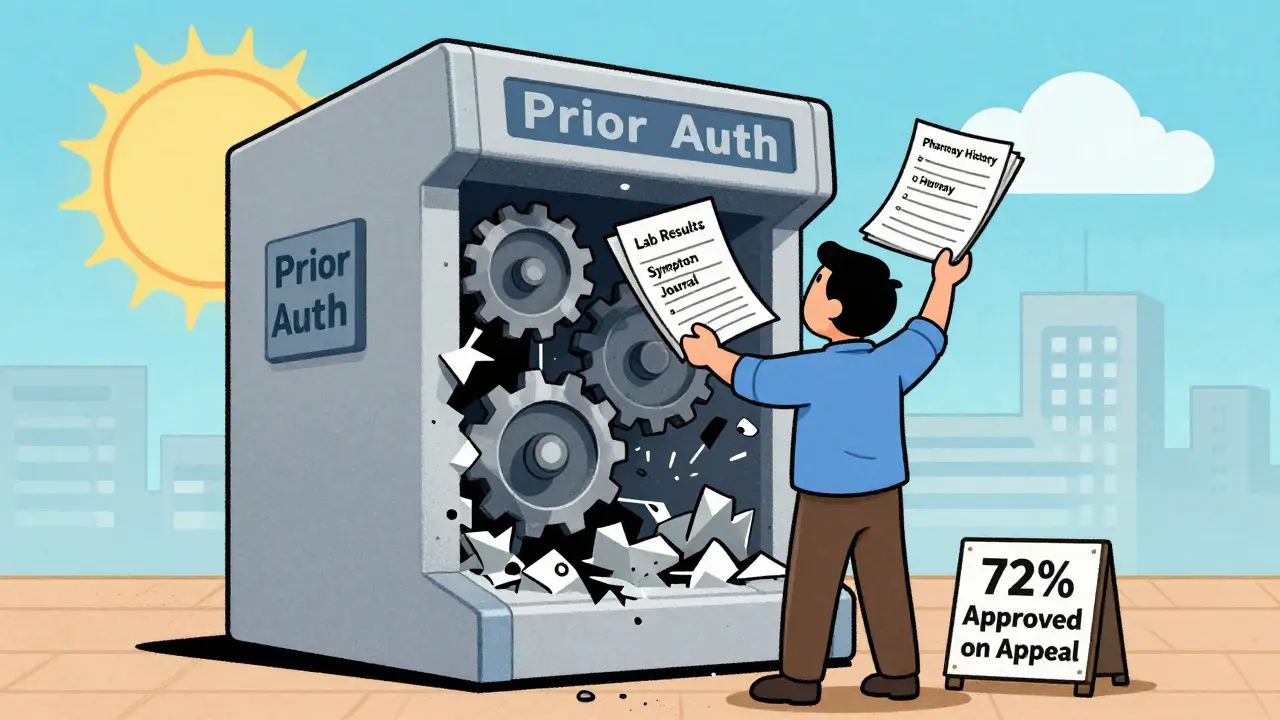
When Brand Is the Only Option
Some drugs don’t have generics at all. Biologics-like Humira, Enbrel, or insulin-are complex molecules that can’t be copied exactly. Instead, there are biosimilars, which are similar but not identical. Many doctors and patients still prefer the original brand because of unpredictable reactions. If you’re on one of these, you’re already in the clear. But if your insurer tries to force you to a biosimilar, you can still appeal. Just like with generics, you need documentation: side effects, loss of symptom control, lab changes.It’s Not About Price-It’s About Control
The system pushes generics because they’re cheaper. That’s not wrong. But your health isn’t a spreadsheet. If a generic makes you feel worse, it’s not a cost-saving-it’s a risk. You have the right to ask for the medication that works for you. You have the right to be heard. And you have the right to bring evidence, not just feelings. You’re not being difficult. You’re being smart.Can I ask my doctor to keep me on brand medication even if a generic is available?
Yes. You have the right to request your preferred medication. Your doctor can write "Dispense as Written" (DAW-1) on the prescription to prevent substitution. They may need to provide documentation-like lab results, symptom logs, or allergy history-to justify it to your insurer, but many doctors will do this if you provide clear evidence.
What if my insurance denies my request for brand medication?
Most denials can be appealed. Your doctor will need to submit clinical documentation showing therapeutic failure with generics, documented allergies to inactive ingredients, or a narrow therapeutic index condition. In the U.S., 72% of these appeals are approved when supported by proper records. In Australia, you can apply for a Special Authority through Medicare or your private insurer. Keep copies of all correspondence and follow up if you don’t hear back in 5-7 days.
Are generic medications really the same as brand-name ones?
For most drugs, yes-they contain the same active ingredient and meet the same safety standards. But for medications with a narrow therapeutic index-like warfarin, levothyroxine, or anti-seizure drugs-even small differences in absorption can affect outcomes. Studies show higher rates of hospital visits and treatment failure in these cases after switching. Inactive ingredients in generics can also cause allergic reactions in sensitive individuals.
How do I know if my medication has a narrow therapeutic index?
Check the FDA’s Orange Book (in the U.S.) or the PBS database (in Australia). Look for the therapeutic equivalence code. If it’s rated AB1 or AB2, it’s considered interchangeable. If it’s rated BX, it means the drug is not recommended for substitution due to potential clinical impact. Common examples include levothyroxine, warfarin, phenytoin, carbamazepine, and cyclosporine. Ask your pharmacist or doctor to confirm.
What if I can’t afford the brand medication even if I need it?
Many pharmaceutical companies offer patient assistance programs for brand-name drugs if you meet income criteria. In Australia, you may qualify for additional subsidies through the PBS Safety Net. In the U.S., organizations like NeedyMeds and RxAssist help connect patients with savings cards and free drug programs. Your doctor or pharmacist can help you apply. Never stop taking your medication because of cost-there are always options to explore.
Next Steps
If you’re thinking about asking your doctor to keep you on brand medication:- Start a symptom journal today-note dates, changes, and how you feel.
- Collect your last three lab results related to your medication.
- Call your pharmacy and ask for a printout of your dispensing history.
- Look up your drug’s therapeutic equivalence rating online.
- Write down three clear reasons why you want to stay on the brand.


Praseetha Pn
January 18, 2026 AT 03:34Okay but have you ever heard of the Big Pharma shadow network? They don’t want you on brand meds because they’re not making enough off the generics-wait, no, that’s not even it. The real story? The FDA’s testing labs are run by the same contractors who audit the generic manufacturers. It’s a closed loop. I saw a whistleblower doc leak last year-some lab tech admitted they tweaked bioequivalence numbers to pass generics that should’ve been BX-rated. And they call it ‘regulatory efficiency.’ 😒
My cousin’s on Lamictal. Switched to generic. Had a seizure during her yoga class. Hospitalized. The pharmacist said, ‘It’s the same thing.’ Same thing? Bro, my cousin’s brain isn’t a spreadsheet.
And don’t get me started on the fillers. One generic had lactose in it. She’s lactose intolerant. They didn’t even list it on the bottle because ‘it’s below the threshold.’ Below the threshold for who? The FDA? Not for her nervous system. This isn’t science-it’s corporate negligence dressed in white coats.
Nishant Sonuley
January 18, 2026 AT 17:16Look, I get it. I really do. I’m a pharmacist in Delhi, been at this for 18 years, and I’ve seen patients crash and burn after switching generics-especially with warfarin and levothyroxine. But let’s not turn this into a superhero origin story where the patient is the lone warrior against Big Pharma. The truth? Most generics are fine. Like, 93% of them. But for the 7% who are sensitive? Yeah, that’s real. And honestly? The system’s broken because we treat meds like widgets.
Here’s what I tell my patients: ‘Don’t just say you feel worse. Show me the numbers. Bring your INR logs. Show me the pill bottles side by side. If your generic looks like a different color candy and you’re getting migraines? That’s not ‘in your head.’ That’s chemistry. And if your doc says ‘it’s the same,’ ask them to look at the FDA’s Orange Book. If it’s AB1, fine. If it’s BX? Then they’re either lazy or lying. Either way, you’re not being difficult-you’re being a good patient.’
Also, side note: if you’re allergic to FD&C Red No. 40 and your generic is neon red? That’s not a coincidence. That’s a red flag. Literally.
Emma #########
January 20, 2026 AT 05:17I had to fight for my brand-name thyroid med for two years. My doctor was so supportive, but the insurance kept denying. I kept sending them my lab results-TSH levels were all over the place after the switch. I kept a journal. I printed out the FDA’s BX rating for levothyroxine. I even called the pharmacy and asked them to confirm the manufacturer changed each time.
Finally, after three appeals, they approved it. I cried. Not because I was ‘spoiled’-because I felt seen. This isn’t about being entitled. It’s about being human. Our bodies aren’t interchangeable. We shouldn’t be treated like they are.
Thank you for writing this. I wish more people understood this.
Andrew Short
January 21, 2026 AT 02:33Wow. Another entitled patient who thinks their body is a magic snowflake that only brand-name pills can touch. Let me guess-you also think your gluten-free, non-GMO, organic, hand-harvested, moon-phase-aligned meds are ‘more effective’?
Generics are FDA-approved. They have the same active ingredient. The 80-125% bioequivalence range? That’s science, not corporate greed. If you’re having side effects, maybe it’s not the pill-it’s your anxiety. Or your diet. Or your sleep. Or the fact that you’re convinced every change is a conspiracy.
And don’t even get me started on ‘inactive ingredients.’ You’re telling me your body can’t handle a trace of lactose but you eat yogurt every morning? That’s not medicine. That’s hypochondria with a spreadsheet.
Stop weaponizing your health. The system’s not broken. You’re just not used to paying less.
Zoe Brooks
January 22, 2026 AT 22:26Thank you for this. 🙏
I’ve been on Keppra for 12 years. Brand. Always. Switched once because my insurance forced it. Had a seizure in the grocery store. My kid saw it. I’ve never felt so powerless.
Now I bring my pill bottles to every appointment. I show them the difference in the coating. The smell. The way the generic dissolves slower. My neurologist says, ‘You’re right. Let’s fight.’
It’s not about being difficult. It’s about being alive. And if that means paperwork? Fine. I’ll do it. Every time.
Kristin Dailey
January 24, 2026 AT 00:55U.S. taxpayers shouldn’t pay for brand drugs when generics exist. Stop whining. Get over it.
Wendy Claughton
January 25, 2026 AT 17:25Okay, I just want to say… I’m so glad someone finally wrote this. 💛
I’ve been on warfarin for 8 years. Switched to generic. My INR went from 2.4 to 4.1 in 3 days. Almost bled out. My doctor was horrified. He said, ‘I didn’t know this could happen.’ And I said, ‘Neither did I… until I almost died.’
Now I keep a folder. Lab results. Pill bottles. Pharmacy receipts. Even a photo of the generic vs. brand side by side. It’s not paranoia. It’s preparation.
And to the person who said ‘it’s all in your head’? Honey, I had a blood clot in my lung. My head is fine. My blood? Not so much.
Thank you for validating what so many of us feel but are too tired to fight for.
Stacey Marsengill
January 25, 2026 AT 23:51So you’re telling me that after years of being told ‘generics are fine,’ you suddenly have a revelation that your body is ‘special’? That’s not science. That’s narcissism wrapped in a lab report.
Everyone else takes generics. Everyone else is fine. Why are you different? Because you’re emotionally attached to the pill’s color? Or the brand name on the bottle?
I’ve been on generic antidepressants for 15 years. No seizures. No crashes. No ‘chemical betrayal.’ You’re not a victim. You’re just someone who doesn’t want to accept that medicine isn’t personalized luxury.
And don’t even get me started on the ‘I brought my pill bottles’ thing. That’s not evidence. That’s performance art.