When your blood calcium stays too high for too long, your body starts eating itself. Not from hunger - from a glitch in your parathyroid glands. These four tiny glands, tucked behind your thyroid in the neck, are supposed to keep calcium balanced. But when they go rogue, they pump out too much hormone, pulling calcium out of your bones, locking it in your kidneys, and flooding your bloodstream. The result? Fatigue that won’t quit, bones that crack under normal stress, and kidney stones that feel like internal knives. This isn’t just aging. This is hyperparathyroidism.
What’s Really Going On Inside Your Body?
Your parathyroid glands act like calcium thermostats. When calcium drops, they release PTH (parathyroid hormone) to pull it from bones, boost absorption in the gut, and tell kidneys to hold onto it. Simple. Efficient. But in primary hyperparathyroidism, one or more glands stop listening. They keep making PTH even when calcium is already sky-high. That’s like a heater that won’t turn off - no matter how hot the room gets. Blood calcium above 10.5 mg/dL (normal is 8.5-10.2) is the red flag. And PTH? It should be low when calcium is high. But in this condition, it’s either normal or high - which is completely wrong. That mismatch is the diagnostic clue doctors look for. Around 85% of cases come from a single benign tumor - an adenoma - on one gland. The rest involve all four glands swelling up (hyperplasia). Cancer? Less than 1%.Why Bone Loss Isn’t Just About Getting Older
You might think thinning bones are just part of aging. But if your calcium’s high and your PTH’s out of control, you’re losing bone 2-4% per year - faster than most postmenopausal women on estrogen therapy. That’s not osteopenia. That’s active bone destruction. Your body’s pulling calcium from your spine and hips to feed a system that doesn’t need it. DXA scans show this clearly: hips, spine, even wrists can drop below the fracture-risk threshold. The numbers don’t lie. People with untreated hyperparathyroidism are 30-50% more likely to break a bone than others their age. And it’s not just fractures. Many patients describe deep, constant bone pain - especially in the back, ribs, or legs - that gets worse over time. Some mistake it for arthritis or fibromyalgia. It’s not. It’s your skeleton being hollowed out from the inside.More Than Just Bones: The Hidden Symptoms
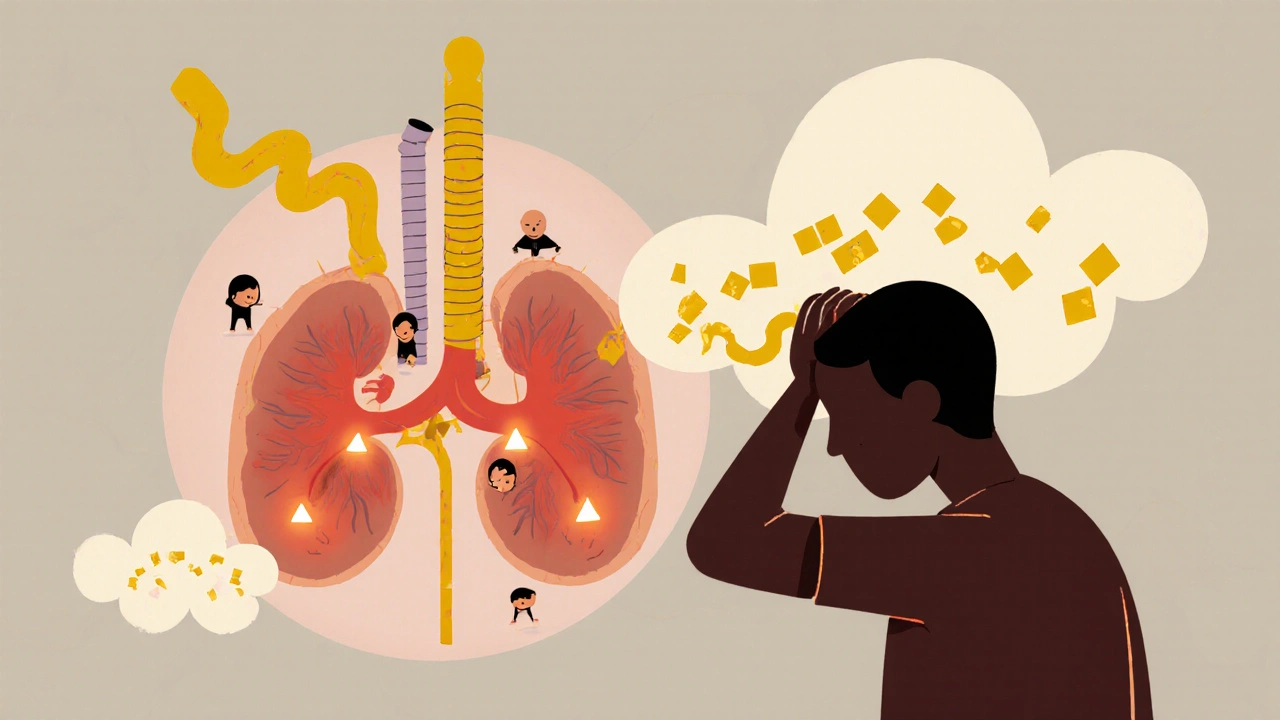
High calcium doesn’t just hurt bones. It messes with your brain, your kidneys, and your energy. Fatigue? It’s not laziness. It’s your cells drowning in calcium. Brain fog? That’s calcium interfering with nerve signals. One patient on a support forum said, “After 7 years of being told I was depressed, my calcium was 11.8 and PTH was 142. After surgery, it felt like someone turned my brain back on.” Kidney stones? Common. Nearly 90% of patients see a drop in stone frequency after surgery. High calcium forces your kidneys to filter more, leaving crystals behind. You might not even notice until it hits you like a brick. And then there’s the nausea, the constipation, the high blood pressure - all tied to calcium overload.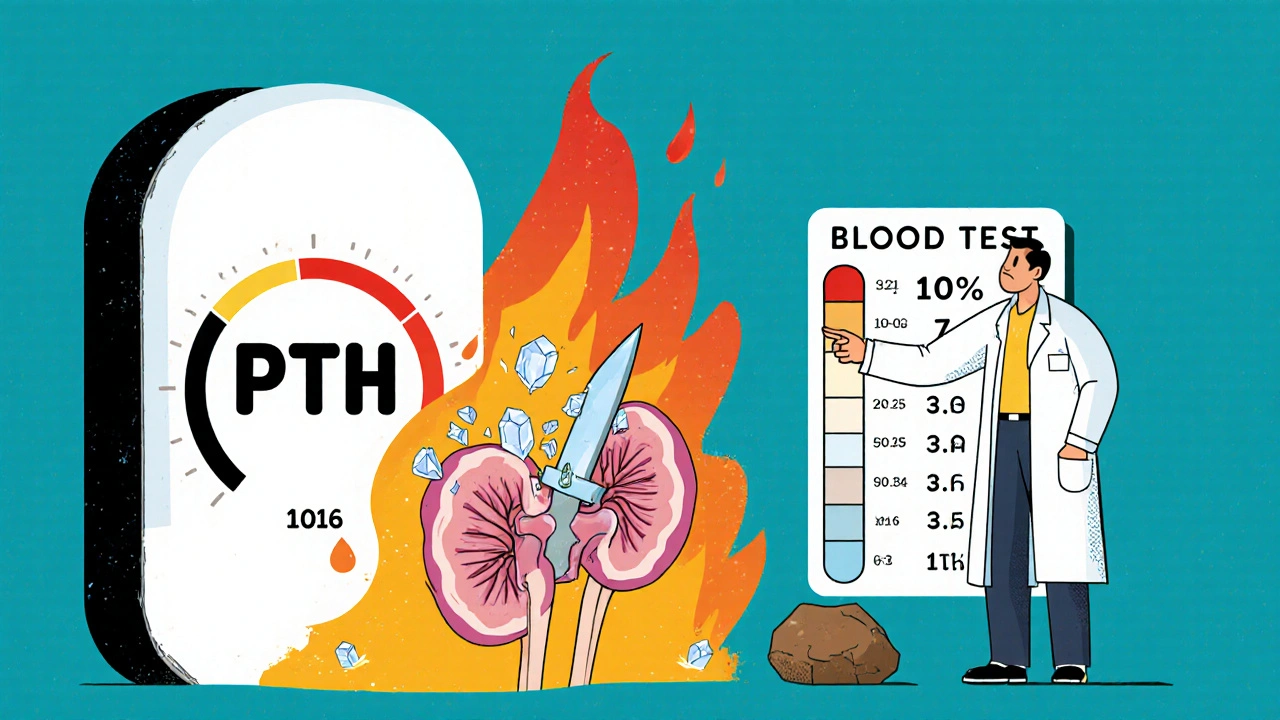
When Is Surgery the Only Real Answer?
Medications can help manage symptoms, but they don’t fix the root problem. Cinacalcet lowers PTH a bit - useful in kidney disease - but only works in 20-30% of primary cases. Bisphosphonates like alendronate can rebuild bone density by 3-5% over two years, but they don’t touch the high calcium. The only cure? Remove the faulty gland(s). The 2022 guidelines say surgery is recommended if you have:- Blood calcium more than 1 mg/dL above the upper limit
- Reduced kidney function (creatinine clearance under 60 mL/min)
- Bone density T-score of -2.5 or worse (osteoporosis)
- Age under 50
What Happens During Surgery?
Minimally invasive parathyroidectomy is now standard. A small incision (1-2 inches), focused on the affected gland. Surgeons use ultrasound and a radioactive tracer (sestamibi scan) to find the problem before cutting. During surgery, they check PTH levels every 10 minutes. If the hormone drops more than 50%, you know the bad gland is gone. Success rate? 95-98% for single-gland disease. The procedure takes about 1-2 hours. Most people go home the same day. Recovery? Usually 3-7 days. You might feel sore in the neck, but the fatigue? That often lifts within days. One patient wrote: “I slept through the night for the first time in 5 years after surgery.”What to Expect After Surgery
Your calcium will drop fast - sometimes too fast. About 30-40% of patients get temporary low calcium (hypocalcemia) after surgery. Your body’s not used to making less PTH. You’ll need calcium supplements - 500-1000 mg three times a day - and sometimes vitamin D (calcitriol) for a few weeks. Most bounce back. But if all four glands were involved, you might need ongoing monitoring for life. Bone density starts improving within a year. By year two, many patients gain 5-8% in spine density. That’s not just a number - it’s fewer fractures, less pain, more mobility.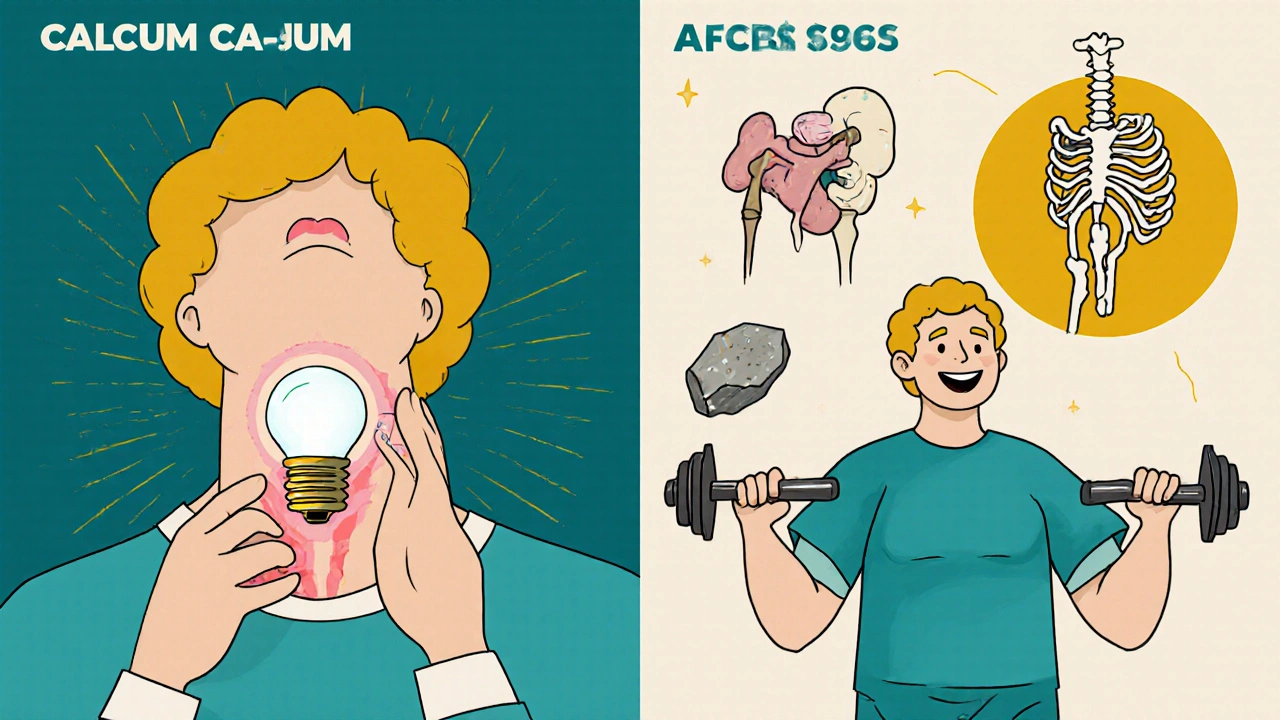
Who Should Avoid Surgery?
Not everyone needs it. If you’re over 50, have mild calcium elevation, normal bone density, and no kidney issues, doctors may suggest watchful waiting. Regular blood tests every 6 months. Annual bone scans. Stay off thiazide diuretics - they make calcium worse. Get enough vitamin D (but don’t overdo it). Walk daily. Strength train. Keep your bones active. But if you’re tired all the time, getting kidney stones, or your bones are thinning - don’t wait. Surgery isn’t risky when done by experienced surgeons. Recurrent laryngeal nerve injury (which can affect voice) happens in less than 1% of cases at high-volume centers. Fear shouldn’t stop you.The Bigger Picture: Why So Many Go Undiagnosed
It’s estimated that nearly half of people with hyperparathyroidism go undiagnosed for years. Why? Symptoms are vague. Fatigue, brain fog, joint pain - all get blamed on stress, depression, or aging. One survey found 47% of patients saw 3+ doctors before getting the right diagnosis. It took them 2-5 years. The good news? Screening is getting better. Medicare now covers routine calcium checks for adults over 65. AI tools are improving scan accuracy. And more surgeons are trained in minimally invasive techniques. The cure rate is high. The recovery is fast. The cost of waiting? Your bones, your energy, your life.Can hyperparathyroidism be cured without surgery?
No, surgery is the only cure for primary hyperparathyroidism. Medications like cinacalcet or bisphosphonates can help manage symptoms or slow bone loss, but they don’t remove the overactive gland. If the root cause isn’t fixed, calcium will keep rising, and bone damage will continue.
How do I know if I have hyperparathyroidism?
It starts with blood tests. If your calcium is consistently above 10.5 mg/dL and your PTH is normal or high, that’s a red flag. A second test a week later confirms it. Doctors may also check vitamin D, kidney function, and bone density. Imaging like ultrasound or sestamibi scans helps locate the problem gland before surgery.
Is parathyroid surgery dangerous?
When done by experienced surgeons, it’s very safe. Complication rates are low: less than 1% risk of voice changes from nerve damage, and less than 5% risk of needing repeat surgery. Most people go home the same day. Temporary low calcium is common but manageable with supplements. The risks of leaving it untreated - fractures, kidney damage, chronic fatigue - are far greater.
Will my bones recover after surgery?
Yes, and often significantly. Bone mineral density typically improves by 3-5% in the first year and up to 5-8% by year two. This happens because your body stops pulling calcium from your skeleton. Weight-bearing exercise and adequate vitamin D help speed recovery. Even if you had osteoporosis, many patients see enough improvement to reduce fracture risk dramatically.
Can hyperparathyroidism come back after surgery?
It’s rare, but possible. If only one gland was removed (most common case), recurrence is 2-3%. If multiple glands were involved, the risk rises to 5-10%. That’s why lifelong annual blood tests are recommended - especially if you had hyperplasia or a family history of endocrine disorders.

Sheldon Bazinga
November 20, 2025 AT 21:10Sandi Moon
November 22, 2025 AT 19:45Kartik Singhal
November 23, 2025 AT 02:22Chris Vere
November 24, 2025 AT 11:38Pravin Manani
November 25, 2025 AT 02:59Mark Kahn
November 26, 2025 AT 09:51Leo Tamisch
November 27, 2025 AT 18:31Daisy L
November 29, 2025 AT 03:51Clifford Temple
November 29, 2025 AT 21:40Corra Hathaway
December 1, 2025 AT 12:46Paula Jane Butterfield
December 2, 2025 AT 01:48Sheldon Bazinga
December 2, 2025 AT 04:34