Introduction to Lupus and Allergies
As someone who has been living with lupus for years, I understand how challenging it can be to manage the various symptoms and complications that come with it. One aspect that often doesn't get enough attention is the connection between lupus and allergies. In this article, I will discuss the link between these two conditions and provide practical advice on how to manage them effectively.
Understanding Lupus and Its Symptoms
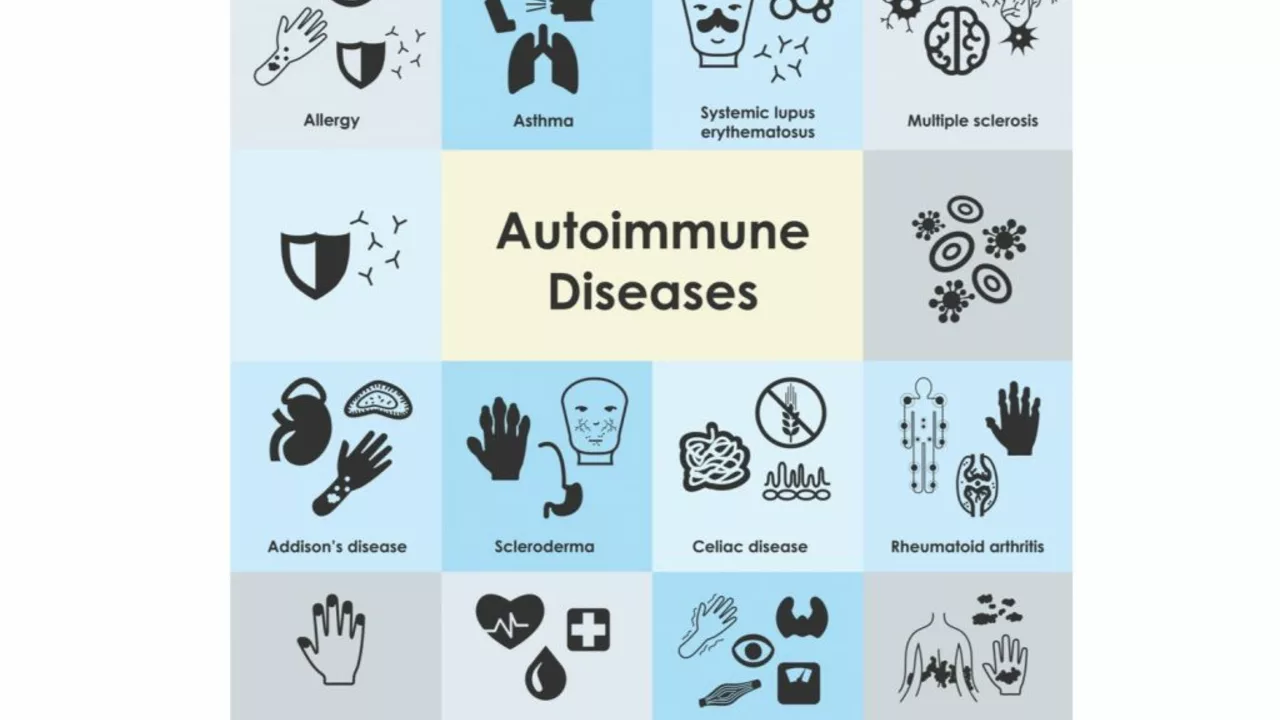
Lupus is an autoimmune disease that causes the immune system to attack healthy tissues, leading to inflammation and damage in various parts of the body. It can affect the skin, joints, kidneys, heart, lungs, and brain. Common symptoms include fatigue, joint pain, skin rashes, and fever. Lupus is a complex condition that affects each person differently, and its symptoms can range from mild to severe.
What Are Allergies?
Allergies are a common condition where the immune system reacts abnormally to certain substances called allergens. These allergens can include pollen, dust mites, pet dander, and certain foods. When the immune system encounters an allergen, it produces an antibody called immunoglobulin E (IgE) which can trigger various symptoms such as sneezing, itching, and wheezing. In some cases, allergies can lead to more severe reactions like anaphylaxis, which can be life-threatening.
The Connection Between Lupus and Allergies
Both lupus and allergies involve the immune system, and it is believed that there is a connection between the two conditions. People with lupus often have an overactive immune system, which can make them more susceptible to developing allergies. In addition, certain medications used to treat lupus, such as corticosteroids, can also increase the risk of allergies.
Managing Allergies in People with Lupus
Effectively managing allergies is crucial for people with lupus, as uncontrolled allergies can exacerbate lupus symptoms and vice versa. Here are some strategies that can help:
1. Identify Your Allergens
The first step in managing allergies is to identify your specific allergens. This can be done through allergy testing, which may include skin prick tests, blood tests, or elimination diets. Once you know your triggers, you can take steps to avoid exposure to them as much as possible.
2. Take Medications as Prescribed
Your healthcare provider may prescribe medications to help manage your allergies, such as antihistamines, decongestants, or corticosteroids. It's essential to take these medications as directed and to communicate any side effects or concerns to your healthcare provider.
3. Use Allergy-Proof Bedding
Using allergy-proof bedding, such as mattress and pillow covers, can help reduce exposure to allergens like dust mites, which can be particularly problematic for people with lupus.
4. Keep Indoor Air Clean
Investing in an air purifier, regularly changing air filters, and keeping windows closed during high pollen days can help reduce the presence of allergens in your home.
How Lupus Medications Can Affect Allergies
As mentioned earlier, some lupus medications, like corticosteroids, can increase the risk of allergies. While these medications can be effective in managing lupus symptoms, they can also suppress the immune system, making it more susceptible to allergens. It's essential to work closely with your healthcare provider to find the right balance of medications to manage both lupus and allergies effectively.
When to Seek Medical Help
If you have lupus and are experiencing allergy symptoms that are not well-controlled with over-the-counter medications or your current treatment plan, it's important to consult your healthcare provider. They can help determine the best course of action, which may include additional testing, adjusting your medications, or referring you to an allergist for specialized care.
Conclusion
Living with lupus and allergies can be challenging, but understanding the connection between the two conditions and taking steps to manage them effectively can significantly improve your quality of life. By working closely with your healthcare provider and implementing the strategies discussed in this article, you can take control of your health and live a more comfortable and fulfilling life.

Louie Lewis
June 18, 2023 AT 15:05The immune labyrinth is a grandiose theater of misdirection.
Eric Larson
June 20, 2023 AT 08:45Wow, this article really hits the nail on the head!!! I mean, who knew lupus could be such a sneaky beast, juggling autoimmunity and allergies like a circus act!!! The writer nailed the connection, and the tips are pure gold!!!
Kerri Burden
June 22, 2023 AT 02:25Lupus, a systemic autoimmune disorder, is characterized by the production of autoantibodies that target nuclear components.
The resultant immune complex deposition precipitates vasculitis and tissue inflammation across multiple organ systems.
Concurrently, atopic sensitization involves IgE‑mediated mast cell degranulation in response to exogenous allergens.
Epidemiological studies have demonstrated a statistically significant comorbidity index between systemic lupus erythematosus (SLE) and allergic rhinitis, asthma, and urticaria.
Pathophysiologically, the dysregulated Th1/Th2 cytokine milieu in lupus patients may predispose to a skewed Th2 response, thereby facilitating IgE class switching.
Moreover, glucocorticoid therapy, while suppressing systemic inflammation, can paradoxically upregulate eosinophil survival, amplifying allergic effector mechanisms.
Clinicians should therefore incorporate comprehensive allergen profiling, such as specific IgE panels or skin prick testing, into routine SLE management protocols.
Environmental control measures, including high‑efficiency particulate air (HEPA) filtration and allergen‑impermeable bedding encasements, have been shown to reduce exacerbation frequency.
Pharmacologically, second‑generation antihistamines with minimal anticholinergic burden are preferred to avoid compounding fatigue, a hallmark lupus symptom.
In refractory cases, adjunctive biologics targeting interleukin‑5 or IgE may offer dual benefit for both disease axes.
Patient education regarding the bidirectional impact of uncontrolled allergy on lupus flare risk is essential for shared decision‑making.
Telemedicine platforms can facilitate longitudinal monitoring of symptom diaries, enabling early intervention.
Research into the shared genetic loci, such as HLA‑DRB1*0301, may elucidate the mechanistic overlap and guide precision therapeutics.
Ultimately, an interdisciplinary approach integrating rheumatology, allergy‑immunology, and dermatology yields the most optimal clinical outcomes.
By proactively addressing allergenic triggers, individuals with lupus can mitigate additive inflammatory burden and preserve quality of life.
Joanne Clark
June 23, 2023 AT 20:05I think the article missed the point that not every1 with lupus gets allergies, lol.
George Kata
June 25, 2023 AT 05:25You raise a good point, Joanne; however, epidemiological data suggests a notable overlap, so it’s worth considering.
Nick Moore
June 26, 2023 AT 17:32Great rundown! Just remember to keep a symptom diary-you’ll spot patterns faster. Also, don’t underestimate the power of a good air purifier.
Jeffery Reynolds
June 28, 2023 AT 08:25While the content is generally accurate, proper grammar demands that we say “people with lupus” rather than “lupus people.” Also, the United States has excellent resources for both rheumatology and allergy care.
Mitali Haldankar
June 29, 2023 AT 20:32Honestly, I think the whole “lupus‑allergy link” is just another pharma ploy 🤔💊. They want us to buy more meds!
snigdha rani
July 1, 2023 AT 00:18Oh sure, because every pharma company loves a good conspiracy 😂. Maybe just try the usual antihistamines first?
Mike Privert
July 2, 2023 AT 09:38Stay consistent with your treatment plan, and don’t hesitate to reach out to your healthcare team if symptoms flare. Small steps lead to big improvements.
Veronica Lucia
July 3, 2023 AT 21:45From a philosophical standpoint, managing two chronic conditions is a reminder of the body’s intricate balance; honoring that balance can be a form of self‑care.
Sriram Musk
July 5, 2023 AT 12:38In practice, integrating allergy testing into the routine SLE work‑up can streamline patient management and reduce redundant appointments.
allison hill
July 6, 2023 AT 19:12But what if the “integration” you mention is just a bureaucratic excuse to keep patients in endless loops of labs? Drama aside, the system often fails us.
Tushar Agarwal
July 8, 2023 AT 04:32Nice insights! Keep it up 😊👍.
Richard Leonhardt
July 9, 2023 AT 16:38Remember, consistency is key – even if you mistype a word now and then. Keep pushing forward, and you’ll see progress.