For millions of people living with chronic or acute pain, opioids have long been the go-to solution. But the risks-addiction, breathing problems, constipation, and tolerance-are too high to ignore. The good news? You don’t need opioids to manage pain effectively. A smarter, safer approach called multimodal pain management is now the standard of care, backed by the CDC, FDA, and leading pain specialists. This isn’t just theory-it’s working in clinics across the U.S. and Australia, helping people get relief without the danger of addiction.
What Is Multimodal Pain Management?
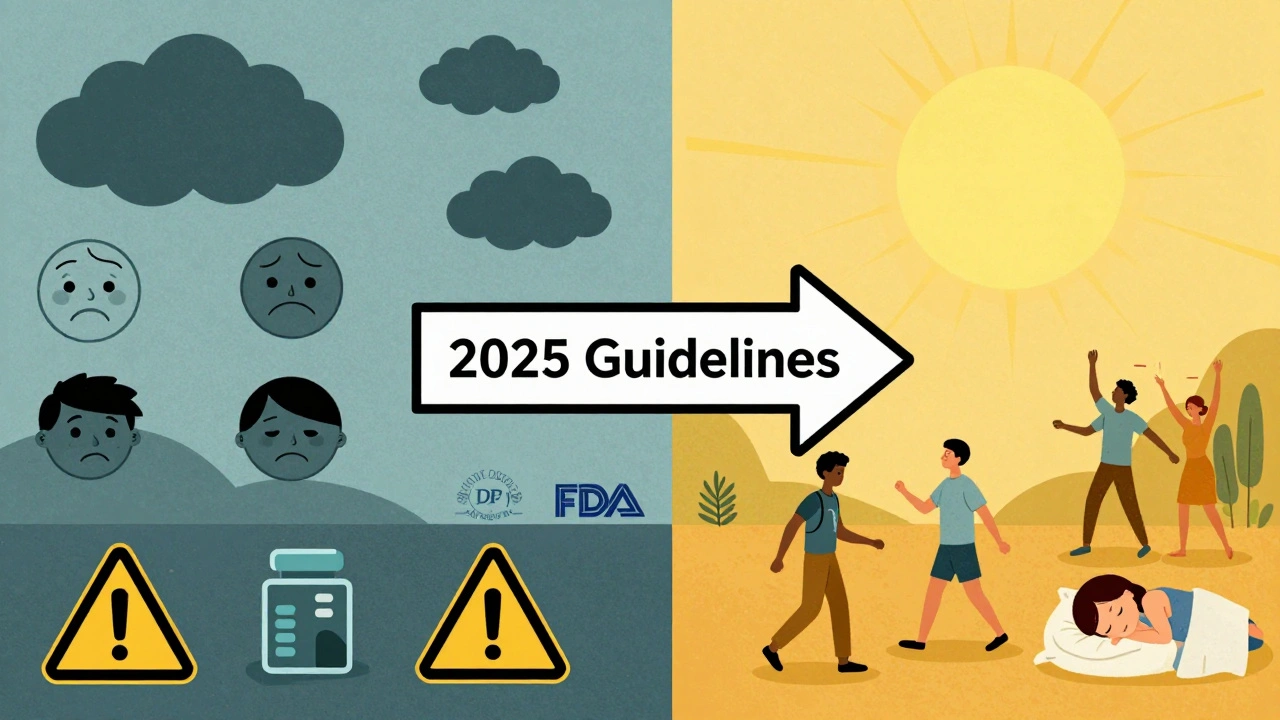
Multimodal pain management means using more than one method at the same time to control pain. Instead of relying on a single drug, it combines non-opioid medications, physical therapies, and mind-body techniques. Think of it like a toolbox: you pick the right tools for the job. For lower back pain, you might use a topical NSAID, do daily stretching, and attend a weekly yoga class. For a sprained ankle, you’d use ice, elevation, and acetaminophen. The goal is simple: reduce pain, improve movement, and avoid opioids entirely.The CDC updated its guidelines in 2022 to make this clear: for chronic or subacute pain, non-opioid treatments should come first. Opioids? Only if everything else fails-and even then, for the shortest time possible. This shift isn’t just policy. It’s based on hard data showing that multimodal approaches work just as well, or better, than opioids for most types of pain-with none of the deadly side effects.
Nonpharmacologic Strategies: Move, Breathe, Heal
You don’t need a pill to ease pain. Movement and mindfulness are powerful tools, especially for long-term conditions like osteoarthritis, fibromyalgia, or lower back pain.Exercise is one of the most effective pain treatments you’ve never been told to try. Regular aerobic activity-like walking, cycling, or swimming-reduces inflammation and boosts natural painkillers in your brain. The CDC recommends 30 to 45 minutes, 3 to 5 days a week. Aquatic therapy in warm water (32-35°C) is especially helpful for joint pain. Resistance training with light weights (60-80% of your one-rep max, 2-3 sets of 8-12 reps) builds muscle that supports sore joints and reduces strain.
Yoga and tai chi combine movement, breath, and focus. Studies show that doing yoga 2-3 times a week for 60-90 minutes reduces chronic pain by 30-50% in many people. Tai chi, done daily for 30-60 minutes, improves balance and reduces pain in arthritis patients. Both are low-cost, low-risk, and can be done at home.
Cognitive behavioral therapy (CBT) doesn’t treat pain directly-it changes how your brain reacts to it. In 8-12 weekly sessions, you learn to recognize negative thought patterns that make pain feel worse. People who complete CBT often report less pain intensity, less anxiety, and better sleep. It’s not “just in your head.” It’s your brain learning new ways to cope.
Acupuncture involves thin needles placed at specific points on the body. Over 8-12 sessions, it can reduce chronic pain by 30-40%. The CDC notes adverse events are extremely rare-only 0.14 per 10,000 treatments. It’s not magic. It likely works by stimulating nerves that block pain signals to the brain.
Nonopioid Medications: What Actually Works
Sometimes, you need something stronger than movement. That’s where nonopioid medications come in-and they’re more effective than many people realize.Topical NSAIDs like diclofenac gel are ideal for localized pain-knee arthritis, muscle strains, or tendonitis. Applied four times a day, they reduce pain by 20-40% with almost no stomach or kidney risks compared to pills. You put it right where it hurts, and it stays there.
Oral NSAIDs like ibuprofen (400-800 mg every 6-8 hours) and naproxen (375-500 mg twice daily) are great for inflammation-based pain. But they’re not for long-term daily use. Taking them for more than a few weeks increases your risk of stomach bleeding by 1-2% per year. Always take them with food, and never mix with alcohol.
Acetaminophen (up to 4,000 mg daily) is safer on the stomach than NSAIDs, but it’s harder on the liver. If you drink alcohol regularly or have liver disease, stick to lower doses. It’s not great for inflammation, but it works well for headaches, mild arthritis, and post-surgery pain.
Tricyclic antidepressants like amitriptyline (10-100 mg at night) are often misunderstood. They’re not for depression here-they’re for nerve pain. Used for conditions like diabetic neuropathy or chronic back pain, they work by calming overactive pain nerves. Side effects include dry mouth and drowsiness, but they’re not addictive.
And then there’s Journavx (suzetrigine). Approved by the FDA in August 2023, it’s the first new non-opioid painkiller in 25 years. It targets a specific nerve channel (NaV1.8) that sends pain signals, blocking them without affecting breathing, cognition, or causing constipation. In clinical trials, it worked as well as opioids for moderate to severe acute pain-like after surgery or a fracture-but without the risk of addiction. This isn’t a miracle drug, but it’s a major step forward.
What Works Best for Different Types of Pain?
Not all pain is the same. The right strategy depends on what’s causing it.Chronic low back pain: Exercise and CBT are the top choices. Studies show 60-70% of people get 30-50% pain reduction after 6-12 weeks of consistent movement and mental training. Topical NSAIDs help for flare-ups. Opioids? They don’t work better-and they’re riskier.
Osteoarthritis (knees, hips): Topical diclofenac gel gives 20-40% pain relief with no system-wide side effects. Daily walking or swimming improves joint function. Weight loss, even just 5-10% of body weight, cuts knee pain in half.
Migraines: Triptans (like sumatriptan) are the gold standard, giving pain freedom in 40-70% of people within two hours. Anti-nausea meds and dihydroergotamine are also effective. Preventive options include magnesium, riboflavin, and CBT to reduce triggers.
Post-surgical or acute injury pain: Ice, elevation, rest, and NSAIDs are the first line. Add acetaminophen for extra relief. For higher pain levels, suzetrigine (Journavx) is now an option. Regional nerve blocks (numbing shots near the injury) are also used in hospitals to avoid opioids entirely.
Nerve pain (neuropathy, shingles): Amitriptyline, gabapentin, or topical lidocaine patches are preferred. New compounds like CP612 (still in research) show promise for chemotherapy-induced nerve pain without addiction risk.
Why This Approach Beats Opioids
Opioids sound powerful-but they come with hidden costs. The CDC reports that 1 in 5 U.S. adults with chronic pain still gets an opioid prescription. That’s dangerous. Every year, 0.7% of chronic pain patients develop an opioid use disorder. That might sound small, but with millions affected, it adds up to tens of thousands of new addictions.Side effects are common: 50-80% of opioid users get breathing problems. 40-95% get severe constipation. Tolerance builds fast-you need more just to feel the same relief. And when the dose goes up, so does the risk of overdose.
Non-opioid methods? They don’t cause addiction. They don’t slow your breathing. They don’t make you constipated. The worst side effect of yoga? Maybe a sore muscle. The worst side effect of acetaminophen? A liver issue-if you take too much. The risks are real, but they’re manageable and far lower.
Even better, some non-opioid treatments get stronger over time. Duke University researchers found that their experimental ENT1 inhibitor compound actually becomes more effective with repeated use. Opioids? They weaken. That’s why people keep increasing their dose. Non-opioid strategies can build resilience, not dependence.
Challenges and Realistic Expectations
This isn’t a quick fix. Multimodal pain management takes time, effort, and consistency.Only 40-60% of people stick with exercise programs for chronic pain. It’s hard to stay motivated when pain flares up. That’s why support matters-group classes, online communities, or a physical therapist who checks in. Low-cost group aerobics can be just as effective as expensive one-on-one PT.
Some non-opioid drugs have risks too. Long-term NSAID use can damage your stomach. Acetaminophen overdose causes liver failure. That’s why dosing matters. Always follow label instructions. Talk to your doctor before combining medications.
And not every pain responds equally. Severe trauma-like a broken bone or major surgery-often needs something stronger than a pill or yoga pose. In those cases, short-term use of opioids may still be necessary. But even then, multimodal approaches can reduce the total opioid dose needed by half or more.
What’s Next in Non-Opioid Pain Relief?
The future is bright. The FDA is actively encouraging faster development of non-opioid drugs. The NIH has poured $1.9 billion into research through the HEAL Initiative. Companies are testing new targets: enzymes like PLA2, sodium channels like NaV1.8, and adenosine pathways.By 2028, experts predict non-opioid treatments will be the first-line choice for 65% of chronic pain cases-up from 45% in 2022. Pain specialists are already ahead of the curve: 73% now use multimodal approaches as their default, compared to just 42% in 2018.
Research is moving fast. CP612, developed at UT Health San Antonio, reduced nerve pain from chemotherapy and eased opioid withdrawal-all without addiction. Duke’s ENT1 inhibitor is ready for human trials in 2-3 years. New guidelines from the CDC are expected in late 2025, likely reinforcing these strategies even further.
This isn’t about replacing one drug with another. It’s about changing how we think about pain. Pain isn’t just a signal-it’s a complex system involving nerves, muscles, emotions, and the brain. Treating it requires more than one tool. It requires a plan.
Getting Started: Your First Steps
If you’re managing pain without opioids, here’s how to begin:- Track your pain: Note when it flares, what makes it better or worse, and how intense it is (1-10 scale).
- Talk to your doctor: Ask if you’re a candidate for non-opioid first-line treatment.
- Start with movement: Walk 20 minutes a day, 5 days a week. Add stretching or yoga twice a week.
- Try a topical NSAID: For joint or muscle pain, apply diclofenac gel daily.
- Consider CBT: Look for a therapist trained in pain management.
- Avoid mixing meds: Don’t take NSAIDs with alcohol or multiple painkillers without checking with your doctor.
You don’t have to do everything at once. Pick one thing. Do it for a month. See how you feel. Then add another. Small steps lead to big changes.
Pain doesn’t have to control your life. With the right tools, you can move better, sleep deeper, and live fuller-without opioids.
Can non-opioid methods really work as well as opioids for severe pain?
Yes-for many types of pain. For acute pain like after surgery, the new drug suzetrigine (Journavx) has shown equal pain relief to opioids without the risk of addiction or breathing problems. For chronic pain like arthritis or back pain, combining exercise, CBT, and topical NSAIDs often leads to 30-50% pain reduction, which is as good as or better than long-term opioid use. Opioids may give stronger short-term relief, but they lose effectiveness over time and carry high risks. Non-opioid methods build lasting improvement.
Are there any non-opioid pain meds that are addictive?
The medications commonly used in non-opioid pain management-like NSAIDs, acetaminophen, topical gels, antidepressants (e.g., amitriptyline), and anticonvulsants (e.g., gabapentin)-are not addictive. They don’t trigger the brain’s reward system like opioids do. However, some people may develop a psychological reliance on pain relief, especially if they’ve used opioids before. That’s why combining medication with movement and mindset strategies (like CBT or yoga) is so important: it reduces dependence on any single treatment.
How long does it take for non-opioid treatments to start working?
It depends. Topical NSAIDs and acetaminophen can work within an hour. Exercise and yoga take weeks to show results-usually 4-8 weeks of consistent effort. CBT typically shows improvement after 6-8 sessions. Acupuncture often needs 6-12 sessions before pain noticeably decreases. The key is patience. Unlike opioids, which mask pain quickly, non-opioid methods rebuild your body’s ability to handle pain. The benefits last longer and come with fewer side effects.
Can I use non-opioid methods if I’ve been on opioids before?
Absolutely. Many people successfully transition off opioids using multimodal approaches. The process usually involves gradually reducing the opioid dose while adding non-opioid treatments like exercise, CBT, and nerve-targeted medications. This is best done under medical supervision to manage withdrawal symptoms and prevent pain rebound. Research shows that combining these strategies improves success rates and reduces the chance of relapse.
What’s the cheapest way to start managing pain without opioids?
Start with walking and over-the-counter acetaminophen. A daily 20-minute walk costs nothing and improves circulation, reduces inflammation, and boosts mood. Acetaminophen (up to 4,000 mg daily) is inexpensive and effective for many types of pain. You can also find free or low-cost yoga videos online or join a community center class for $10-20 per session. Topical diclofenac gel is available over the counter in many countries and is often cheaper than daily opioid prescriptions. Small, consistent actions make the biggest difference.
Is there a risk of overusing non-opioid medications like NSAIDs?
Yes. Long-term daily use of NSAIDs (like ibuprofen or naproxen) can cause stomach ulcers, kidney damage, or high blood pressure. The risk is about 1-2% per year with regular use. To reduce risk: take the lowest effective dose, use them only when needed, avoid alcohol, and never take more than one NSAID at a time. For chronic pain, focus on non-drug methods and use NSAIDs only for flare-ups. Topical versions are much safer than pills.
Where can I find a provider who specializes in non-opioid pain management?
Look for pain clinics that emphasize multidisciplinary care-meaning they include physical therapists, psychologists, and doctors trained in non-opioid strategies. Ask your primary care doctor for a referral. Professional organizations like the American Society of Anesthesiologists and the American Society of Regional Anesthesia have directories of certified providers. In Australia, look for clinics affiliated with hospitals or universities that follow the latest CDC and international guidelines. Avoid providers who push opioids as the main solution.


Paul Corcoran
December 2, 2025 AT 15:56Finally someone’s talking sense. I’ve been doing yoga and walking every day for my back pain, and honestly? It’s changed my life. No more pills, no more dread of side effects. Just movement, breath, and patience. It’s not magic, but it’s real.
Start small. Even 10 minutes a day adds up. You don’t need a gym or a prescription. Just show up.
Chris Jahmil Ignacio
December 3, 2025 AT 14:23Yeah right. Multimodal this. Multimodal that. You think the pharmaceutical industry just let this happen because they care about your health? Wake up. This is a slow rollout to phase out opioids so they can push their new synthetic painkillers under the radar. Journavx? Sounds like a brand name for a controlled substance with a new label. The CDC? FDA? All bought and paid for. They want you dependent on their new drugs, not yoga. Watch the timeline. This is corporate control disguised as wellness.
And don’t get me started on acupuncture. Needles? Really? That’s science now? Tell me how many double-blind studies actually prove it’s not placebo. Spoiler: they don’t. But you’ll believe anything if it sounds holistic.
Colin Mitchell
December 3, 2025 AT 14:54Hey Chris, I hear you. I used to think the same thing - that pain meant pills. But after my knee surgery, my PT pushed me to try ice, elevation, and acetaminophen instead of opioids. I was skeptical. But after two weeks, I realized I wasn’t just avoiding addiction - I was actually healing better. No foggy brain. No constipation. Just me, moving again.
It’s not about rejecting medicine. It’s about choosing smarter tools. And yeah, yoga feels weird at first. But try it for 10 minutes. You might be surprised.
Stacy Natanielle
December 4, 2025 AT 09:19Okay, but let’s be real - this article is dangerously oversimplified. 🤨
Acetaminophen? Liver failure is no joke. NSAIDs? GI bleed risk is statistically significant. CBT? Only works if you’re psychologically stable - which most chronic pain patients are NOT. And suzetrigine? Phase 3 trials had 12% dropout rate due to dizziness. This reads like a pharma ad disguised as public health advice. Where’s the nuance? Where’s the data on long-term adherence? Where’s the disclaimer that 60% of people quit exercise within 3 months?
Also - why is everyone ignoring the fact that this approach is inaccessible to low-income communities? Yoga mats don’t grow on trees. 🤷♀️
kelly mckeown
December 5, 2025 AT 00:04i just wanted to say… thank you for writing this. i’ve been in chronic pain for 8 years and opioids made me feel like a ghost. i started walking every morning and it’s been hard, but i’m sleeping better. not perfect, but better. i still have bad days. but now i don’t feel like i’m losing myself to the meds. just… thank you.
ps: i typoed half this comment. sorry. 😅
Tom Costello
December 6, 2025 AT 16:49Good breakdown. One thing missing: access. Not everyone lives near a physical therapist or can afford a CBT therapist. Community centers, free online yoga channels, and local libraries offering pain management workshops are the real unsung heroes here.
Also, the idea that ‘non-opioid = no drugs’ is misleading. Amitriptyline isn’t a candy. It’s a medication with side effects. But it’s not addictive. That’s the key distinction. We need to stop framing this as ‘drugs bad, yoga good.’ It’s ‘right tool, right time.’
dylan dowsett
December 6, 2025 AT 19:17Wait - you’re seriously telling people to skip opioids for post-surgical pain?!!
Have you ever had a hip replacement? Or a broken femur? You think yoga is going to help when you can’t even move your leg?! This is dangerous. People are going to suffer needlessly because some blogger thinks they’re being ‘responsible.’
And don’t get me started on ‘Journavx’ - it’s literally just a new opioid with a different name. They just changed the chemical structure to bypass patent laws. I’ve seen the FDA documents. They’re hiding the addiction potential. Don’t be fooled.
Also - why is no one talking about how this is just another way to deny pain patients real relief? It’s not empowerment. It’s neglect.
Susan Haboustak
December 7, 2025 AT 10:04Let’s not romanticize this. The article cherry-picks data. CBT doesn’t work for 70% of people with fibromyalgia - it works for maybe 30%, and only if they’re already high-functioning. Acupuncture? The mechanism is unproven. Topical NSAIDs? Fine for knees. Useless for neuropathic pain. And suzetrigine? Phase 2 trials showed no difference from placebo in patients over 65.
Also - the CDC guidelines are based on observational studies, not RCTs. You can’t make population-wide policy on weak evidence. And the fact that this is being pushed as ‘standard of care’ without addressing socioeconomic barriers is unethical. This isn’t medicine. It’s performative wellness.
Chad Kennedy
December 8, 2025 AT 15:21Ugh. More of this ‘just walk it off’ nonsense. I’ve got sciatica. I can’t walk. I can barely sit. You think yoga is gonna fix that? Nah. I need something that works NOW. Not in 6 weeks. Not after I’ve spent $200 on a mat I’ll never use.
And who even wrote this? Some guy who’s never had real pain? I’ve been on opioids for 5 years. Yeah, I’m dependent. But I’m functional. I work. I take care of my kids. You want me to quit? Fine. But give me something that doesn’t leave me crying on the floor.
This whole post feels like guilt-tripping people who are just trying to survive.
Siddharth Notani
December 9, 2025 AT 21:10Excellent overview. In India, we have a long tradition of Ayurvedic pain management - turmeric, ginger, massage, and meditation. These are not ‘alternative’ - they are foundational. The science behind them is emerging, and it aligns with multimodal approaches.
For example, curcumin has been shown in multiple RCTs to reduce inflammation comparable to ibuprofen, with no GI risk. And in rural clinics, group walking programs have reduced chronic pain by 40% over 6 months.
Western medicine is catching up. But the wisdom was always there.
Cyndy Gregoria
December 11, 2025 AT 19:12YOU CAN DO THIS. I was in the same place as Chad. I thought opioids were my only option. I started with 10-minute walks. Then I added stretching. Then I found a free CBT app. It took 3 months. But now? I’m off opioids. I sleep. I laugh. I hike. It wasn’t easy. But it was worth it.
Start with ONE thing today. Not tomorrow. TODAY. You’ve got this. 💪❤️
Akash Sharma
December 12, 2025 AT 03:15This is fascinating. I’ve been researching pain pathways for my thesis, and what’s missing here is the neuroplasticity angle. Chronic pain isn’t just a signal - it’s a rewired circuit. That’s why CBT and movement work: they literally reshape the brain’s pain map. Studies from Stanford and MIT show that after 8 weeks of mindfulness + exercise, the anterior cingulate cortex - the area that processes pain intensity - shows measurable thinning in activity.
Also, the mention of ENT1 inhibitors is huge. That’s a new class of analgesics that modulate endocannabinoid signaling without CB1 activation - meaning no psychoactive effects. If this works in humans, it could be the first non-addictive, non-opioid, non-NSAID analgesic that actually reverses central sensitization. That’s not just an alternative - it’s a paradigm shift.
And yes, the timeline matters. Most people give up before week 4. But if you stick past 6 weeks, your nervous system starts adapting. The pain doesn’t disappear - but your tolerance for it increases. That’s the real win.
Justin Hampton
December 12, 2025 AT 17:01Everyone’s acting like this is some revolutionary breakthrough. Newsflash: we’ve known this stuff for decades. The problem isn’t the science. It’s the system. Insurance won’t cover CBT. Physical therapy is capped at 10 visits. Yoga studios are expensive. Acupuncture? Cash only. Meanwhile, opioids? Covered. Prescribed in 5 minutes. No follow-up.
This article is just pretty words for a broken system. The real issue isn’t that people don’t know what works. It’s that the system won’t let them access it.
So no. This isn’t a solution. It’s a distraction.