Diarrhea is one of those things no one talks about until it hits - and then you’re scrambling for the nearest bathroom and the closest medicine cabinet. You’ve got three or four loose stools in a day, cramps, maybe some nausea. You reach for Imodium or Pepto-Bismol because they’re right there, cheap, and you’ve used them before. But here’s the thing: OTC diarrhea treatments aren’t magic pills. They’re tools. And like any tool, using them wrong can make things worse.
What’s Actually in These Pills?
There are two main types of OTC diarrhea meds you’ll find on any pharmacy shelf: loperamide and bismuth subsalicylate. That’s Imodium and Pepto-Bismol, respectively. They work in totally different ways.Loperamide slows down your gut. It’s a synthetic opioid, but don’t worry - at normal doses, it doesn’t affect your brain. It just binds to receptors in your intestines and tells them to chill out. That means food moves slower, water gets reabsorbed, and you’re not running to the bathroom every 20 minutes. Studies show it cuts stool frequency by up to 62% within 24 hours. It kicks in within 30 to 60 minutes. If you’re stuck on a plane or in a meeting, this is your go-to.
Bismuth subsalicylate - the active ingredient in Pepto-Bismol - does more than just slow things down. It coats your gut like a bandage, mops up toxins, reduces inflammation, and even kills some of the bacteria causing the problem, like E. coli and Campylobacter. It’s also the only one that helps with nausea and stomach cramps. That’s why people swear by it for traveler’s diarrhea. But there’s a catch: it turns your stool black and your tongue gray. It’s harmless, but if you don’t know it’s normal, you’ll panic.
When It’s Safe to Use Them
If you’re otherwise healthy and your diarrhea started suddenly - maybe after a bad taco or a new kind of yogurt - and you’re not running a fever, then yes, OTC meds are fine. The goal isn’t to stop diarrhea completely. It’s to give your body time to fight off the bug without getting dehydrated or exhausted.The American College of Gastroenterology says most cases of acute diarrhea resolve on their own in 5 to 7 days. You’re not curing anything. You’re just making it bearable. Use loperamide: take 4mg after the first loose stool, then 2mg after each one after that. Don’t go over 8mg in 24 hours. For Pepto-Bismol, take 30mL (two tablespoons) after each loose stool, up to 8 doses in 24 hours. That’s about 1,000mg of bismuth subsalicylate max.
Hydration matters more than the pill. Drink fluids with electrolytes - not just water. WHO-recommended oral rehydration solutions have the right balance of salt and sugar. If you don’t have those, mix 1 liter of water with 6 teaspoons of sugar and half a teaspoon of salt. Sip it slowly. Avoid milk, caffeine, alcohol, and high-fiber foods. Stick to the BRAT diet: bananas, rice, applesauce, toast. They’re bland, easy to digest, and help firm up stools.
When You Should NOT Use Them
This is where most people mess up. Don’t take loperamide or Pepto-Bismol if you have:- Fevers over 100.4°F (38°C)
- Bloody or black, tarry stools
- Severe abdominal pain or swelling
- Diarrhea lasting more than 48 hours
Why? Because diarrhea is your body’s way of flushing out bad stuff. If you’re fighting a bacterial infection like Salmonella or Shigella, slowing your gut down with loperamide can trap those bacteria inside. That’s how you get complications like toxic megacolon - a life-threatening swelling of the colon. The CDC says 15-20% of infectious diarrhea cases involve fever or blood. If you’ve got either, skip the OTC meds and call a doctor.
Pepto-Bismol contains salicylate - the same compound as aspirin. Don’t give it to kids under 12, and never use it if you’re allergic to aspirin. It can cause Reye’s syndrome in children, a rare but deadly condition. Also, if you’re on blood thinners or have kidney disease, check with a pharmacist first. Bismuth can build up and cause toxicity.

What the Experts Warn About
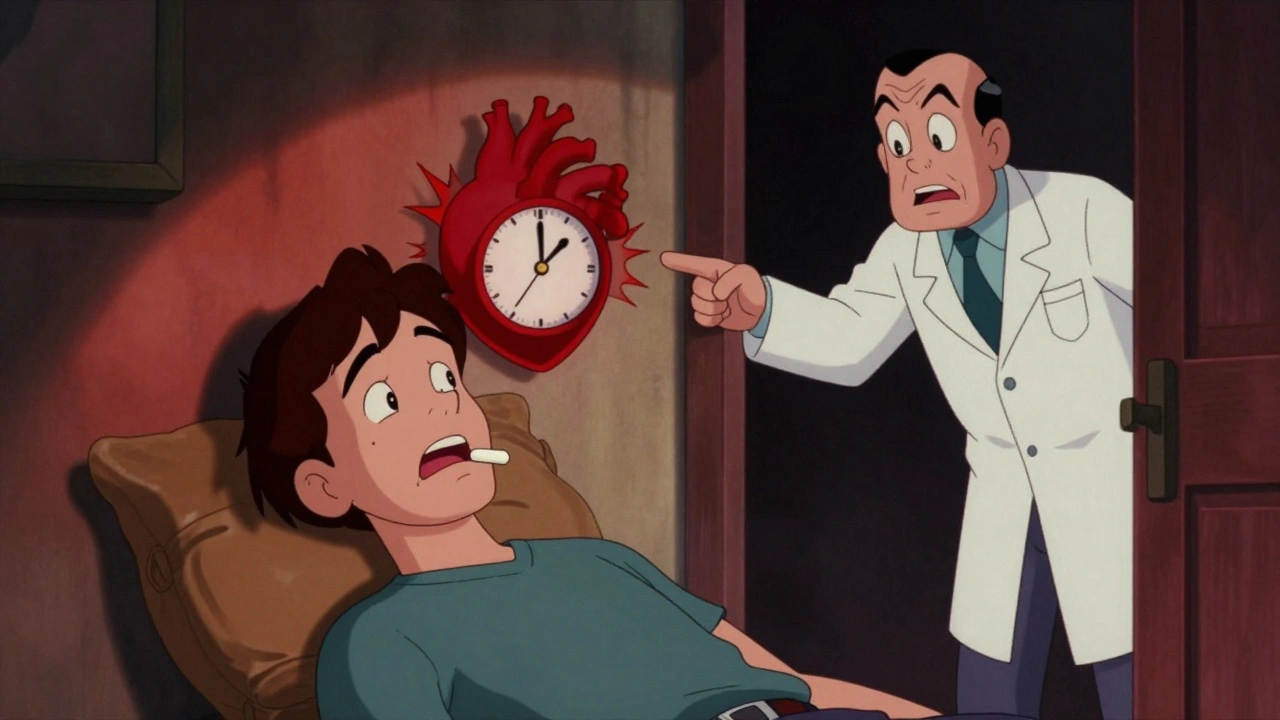
The FDA issued a safety alert in 2016 after 48 deaths linked to loperamide abuse. People were taking 50, 100, even 200mg a day to self-treat opioid withdrawal. That’s 25 to 50 times the recommended dose. At those levels, loperamide crosses the blood-brain barrier, causes heart rhythm problems, and can stop your heart. There are documented cases of people ending up in the ER with QT prolongation - a dangerous heart rhythm - because they thought more was better.Doctors at Massachusetts General Hospital report seeing patients who’ve been using loperamide for months, thinking it’s harmless. One Reddit user wrote: “I took 6 caplets in 4 hours - ended up in the ER with severe constipation.” That’s not an outlier. The FDA’s adverse event database shows nearly 20% of OTC diarrhea medication problems come from overdosing.
And here’s another myth: combining loperamide and Pepto-Bismol. Don’t. You’re doubling down on side effects. Loperamide slows your gut. Pepto-Bismol coats it. Together, they can cause dangerous constipation or salicylate toxicity. Pick one. Use it right. Stop when it’s done.
Who Should Always See a Doctor
Some cases aren’t for self-treatment. You need medical help if:- You’re passing more than six loose stools a day for over 48 hours
- You’re not peeing regularly - less than 0.5mL per kg of body weight per hour
- You’ve lost more than 5% of your body weight in a few days
- You’re over 65, pregnant, or have a weakened immune system
- You’ve recently traveled overseas or taken antibiotics
These aren’t just “be careful” warnings. They’re red flags. In older adults, even mild dehydration can trigger kidney failure or heart issues. In kids, diarrhea kills more than you think - mostly from dehydration. If your child has diarrhea and won’t drink, has dry lips, or cries without tears, get help immediately.
Travelers’ diarrhea is common - up to 50% of people visiting developing countries get it. But if it lasts more than 72 hours, or you’re vomiting, feverish, or bloody, you might need antibiotics. OTC meds won’t fix that. A doctor can test your stool and prescribe the right treatment.
What Works Better Than Pills
Here’s the truth: hydration, rest, and time are your best treatments. OTC meds are nice to have, but they’re not essential. In fact, the American College of Emergency Physicians now advises against routinely giving anti-diarrheals in ERs. Why? Because rehydration - fluids, electrolytes, time - works better and safer.Studies show that people who focus on drinking oral rehydration solutions recover just as fast as those who take loperamide, but with far fewer complications. You don’t need to be embarrassed about your symptoms. You need to be smart about them.
And if you’re worried about getting diarrhea on your next trip? Take Pepto-Bismol before meals. A 2022 study in the Journal of Travel Medicine found it cuts your risk by 65% when taken prophylactically. That’s the only time it’s okay to use it preventively.
What to Do Next
If you’ve got mild diarrhea and no warning signs: grab one OTC option, stick to the label, hydrate hard, and rest. You’ll feel better in 24 to 48 hours.If you’ve got any red flags - fever, blood, pain, no improvement after two days - stop the meds. Call your doctor. Go to urgent care. Don’t wait. Diarrhea isn’t always just a stomach bug. It can be a sign of something serious.
And if you’ve ever thought, “I’ll just take a few more pills to make it stop,” stop that thought right now. More is not better. It’s dangerous.
Can I give loperamide to my 8-year-old?
No. Loperamide is only FDA-approved for children 12 and older in caplet form. The liquid form is approved for kids 6 and up, but only under a doctor’s supervision. Children are more sensitive to its effects, and overdosing can cause paralytic ileus - a dangerous stoppage of bowel movement. Never give adult doses to kids. If your child has diarrhea, focus on hydration with oral rehydration solutions and call a pediatrician if it lasts more than 24 hours or if they show signs of dehydration.
Is Pepto-Bismol safe during pregnancy?
It’s not recommended. Pepto-Bismol contains bismuth subsalicylate, which is related to aspirin. Aspirin use during pregnancy, especially in the third trimester, is linked to complications like premature closure of the fetal ductus arteriosus and low amniotic fluid. While occasional use in early pregnancy may not be harmful, it’s best to avoid it. For diarrhea during pregnancy, stick to hydration, the BRAT diet, and talk to your OB-GYN before taking anything.
Why does my stool turn black after taking Pepto-Bismol?
That’s normal. Bismuth reacts with sulfur in your digestive tract to form bismuth sulfide, a black compound. It’s harmless and temporary. Your stool and tongue may turn black or gray, and your urine might darken too. This happens in 98% of users. It’s not bleeding or internal damage. Just a side effect. If you’re unsure whether it’s the medicine or actual blood, call a doctor. But if you’ve just taken Pepto-Bismol and your stool is black, it’s likely the drug.
Can I use OTC diarrhea meds for chronic diarrhea?
No. Chronic diarrhea - lasting more than 4 weeks - isn’t an infection. It could be IBS, Crohn’s disease, celiac disease, or a medication side effect. OTC anti-diarrheals mask symptoms but don’t fix the root cause. Using them long-term can delay diagnosis and lead to complications. If you’ve had loose stools for more than a month, see a doctor. Blood tests, stool cultures, and possibly a colonoscopy may be needed.
What’s the difference between Imodium and generic loperamide?
There’s no difference in the active ingredient. Generic loperamide contains the same 2mg or 4mg of loperamide hydrochloride as Imodium. The only differences are price, brand name, and sometimes inactive ingredients like fillers or coatings. Generic versions are just as effective and often cost half as much. Check the label for the active ingredient - if it says loperamide hydrochloride, it’s the same drug. You don’t need to pay extra for the brand.
How long should I wait before seeing a doctor if OTC meds don’t work?
If your diarrhea hasn’t improved after 48 hours of using OTC meds correctly, it’s time to see a doctor. If you’ve had more than six stools a day, feel dizzy, have a fever over 101.3°F, or notice blood, don’t wait - go now. Even if you’re not sure, it’s better to get checked. Many serious infections like C. difficile or giardiasis need specific treatments that OTC meds can’t provide.


Webster Bull
December 12, 2025 AT 10:09Diarrhea’s just your gut screaming for a vacation. I used to pop Imodium like candy until I learned it’s not a cure-it’s a pause button. Now I hydrate, rest, and let my body do its thing. Less pills, more peace.
Bruno Janssen
December 12, 2025 AT 14:50I hate when people treat diarrhea like it’s no big deal. I had C. diff once. Took me six months to recover. Don’t be that guy.
Tommy Watson
December 14, 2025 AT 09:19OMG I JUST TOOK 6 IMODIUM BECAUSE I WAS ON A PLANE AND NOW I CAN’T MOVE AND MY STOMACH FEELS LIKE A ROCK?? IS THIS WHAT HAPPENS WHEN YOU’RE A GROWN ASS ADULT??
Karen Mccullouch
December 15, 2025 AT 10:30USA best country for meds. Everyone else in the world just suffers. Pepto-Bismol saved my life during my Mexico trip. If you don’t use it, you’re weak. 🇺🇸💪
sharon soila
December 16, 2025 AT 19:00Hydration is the most important thing. Water alone is not enough. You need the right balance of electrolytes. Simple science, but so many forget it. Your body knows what it needs. Listen to it.
nina nakamura
December 18, 2025 AT 01:40Loperamide abuse is a joke. People think they’re smart taking 50mg because they read a Reddit post. You’re not a chemist. You’re not a doctor. You’re just a person who wants to feel better. Stop. Now.
Cole Newman
December 19, 2025 AT 18:04Bro I took Pepto and Imodium together once because I was paranoid. Ended up stuck on the toilet for 3 hours with zero results. Don’t be me. Pick one. Live.
Casey Mellish
December 21, 2025 AT 04:18In Australia, we call it the runs. And yeah, we use Pepto too. But here’s the thing - we also know when to sit still and let nature take its course. No rush. No panic. Just water, rest, and patience. It’s not a race.
Tyrone Marshall
December 21, 2025 AT 20:37For anyone new to this: diarrhea isn’t your enemy. It’s your body’s way of saying, ‘Hey, something’s off - let me fix it.’ OTC meds are like training wheels. They help you ride, but they don’t teach you how to bike. Learn to listen.
Alvin Montanez
December 22, 2025 AT 03:28Let me just say this: if you’re taking OTC meds for more than 48 hours, you’re not managing your health - you’re avoiding reality. You think you’re being smart? You’re just delaying the inevitable. Go see a doctor. It’s not weak. It’s responsible.
Hamza Laassili
December 22, 2025 AT 16:17PEPTO BISMOL TURNS YOUR TONGUE GRAY?? I THOUGHT I WAS DYING. I CALLED 911. IT WAS JUST THE DRUG. I’M SO EMBARRASSED. BUT ALSO… THANKS FOR THE WARNING.
Rawlson King
December 23, 2025 AT 04:35People treat diarrhea like it’s a joke. My cousin died from dehydration after ignoring it for days. Don’t be a statistic. Drink water. Stop the meds. Call someone.
Constantine Vigderman
December 23, 2025 AT 20:31Just got back from Bali and got the runs 😅 Took Pepto before every meal and it saved me! 65% less chance? YES PLEASE. Also, hydration > pills. Always. 💪💧
Jamie Clark
December 24, 2025 AT 14:17You call that a safety alert? 48 deaths? That’s nothing. The real problem is that people are too lazy to learn how their bodies work. You don’t need a doctor to tell you not to overdose. You need common sense. And most people don’t have it.
Sheldon Bird
December 26, 2025 AT 12:02For anyone reading this and feeling ashamed: you’re not alone. Everyone gets the runs. What matters is how you handle it. Stay calm. Hydrate. Don’t panic. And if you’re unsure? Call your doctor. No shame in that. You’re doing better than you think.