Every year, thousands of people die not from taking one drug, but from mixing them. It’s not always illegal substances - often, it’s prescription pills taken with alcohol, or over-the-counter meds combined with antidepressants. The danger isn’t always obvious. You might think, "I’ve had one drink with my painkiller before," or "I’ve taken Xanax with a beer and been fine." But the body doesn’t work that way. Some combinations don’t just add up - they multiply. And the results can be deadly.
Why Some Drug Mixes Are Deadlier Than Others
Not all drug interactions are the same. Some cause mild nausea or dizziness. Others shut down your breathing. The deadliest combinations involve drugs that affect the same system in your body - especially the central nervous system (CNS). When two CNS depressants are taken together, they don’t just make you sleepy. They can slow your breathing so much that your brain stops telling your lungs to work. That’s how someone can go to bed after a few drinks and a pain pill, and never wake up.
Alcohol and opioids are one of the most common lethal pairs. Oxycodone, hydrocodone, fentanyl - these are all opioids. When mixed with alcohol, they increase the risk of respiratory depression by 4.5 times compared to using either alone. The National Institute on Alcohol Abuse and Alcoholism found that alcohol-medication interactions cause 20% of all emergency room visits due to drug side effects. And it’s not just heavy drinkers. Even one or two drinks can push someone over the edge, especially if they’re not used to the medication.
The Opioid and Benzodiazepine Killer Combo
If you’ve been prescribed an opioid for pain and a benzodiazepine like Xanax or Valium for anxiety, you’re at serious risk. The Substance Abuse and Mental Health Services Administration (SAMHSA) found that in 2020, 30.1% of opioid-related overdose deaths also involved benzodiazepines. That’s nearly one in three. These drugs work together to depress the brainstem - the part that controls breathing and heart rate. When both are present, the body loses its ability to respond to low oxygen levels. The result? Slow, shallow breathing that stops entirely.
Doctors used to prescribe these together all the time. But after years of data showing how deadly this combo is, the Centers for Medicare & Medicaid Services (CMS) started requiring electronic alerts in 2019. Pharmacies now flag these prescriptions. Still, 3.2 million Americans were taking both in 2022 - a 15% increase since 2019. If you’re on either of these, don’t assume you’re safe. Talk to your doctor about alternatives. There are safer ways to manage pain and anxiety without stacking these risks.
The Speedball: Cocaine and Heroin - A Deadly Push-Pull
There’s a myth that mixing stimulants and depressants balances each other out. That’s not true. The combination of cocaine and heroin - known as a "speedball" - is one of the most dangerous drug mixes ever documented. The National Institute on Drug Abuse (NIDA) reported that in 2021, 50% of cocaine overdoses involved heroin. It’s not just about addiction. It’s about physiology.
Cocaine speeds up your heart and raises your blood pressure. Heroin slows your breathing and lowers your heart rate. Your body gets conflicting signals. Your heart races while your lungs struggle. This puts immense stress on your cardiovascular system. Acute cases show blood pressure spikes to 180/110 mmHg and heart rates between 110-160 bpm. Many users report blurred vision, paranoia, and seizures before collapse. The CDC confirms this combo is behind many high-profile overdose deaths, including celebrities like River Phoenix and John Belushi.
And here’s the worst part: users often don’t realize how little of either drug it takes to kill them. Fentanyl contamination makes this even more unpredictable. The DEA says 6 out of 10 counterfeit pills now contain a lethal dose of fentanyl. So even if you think you’re taking "heroin," you might be getting something far stronger - and mixing it with cocaine? That’s a death sentence.
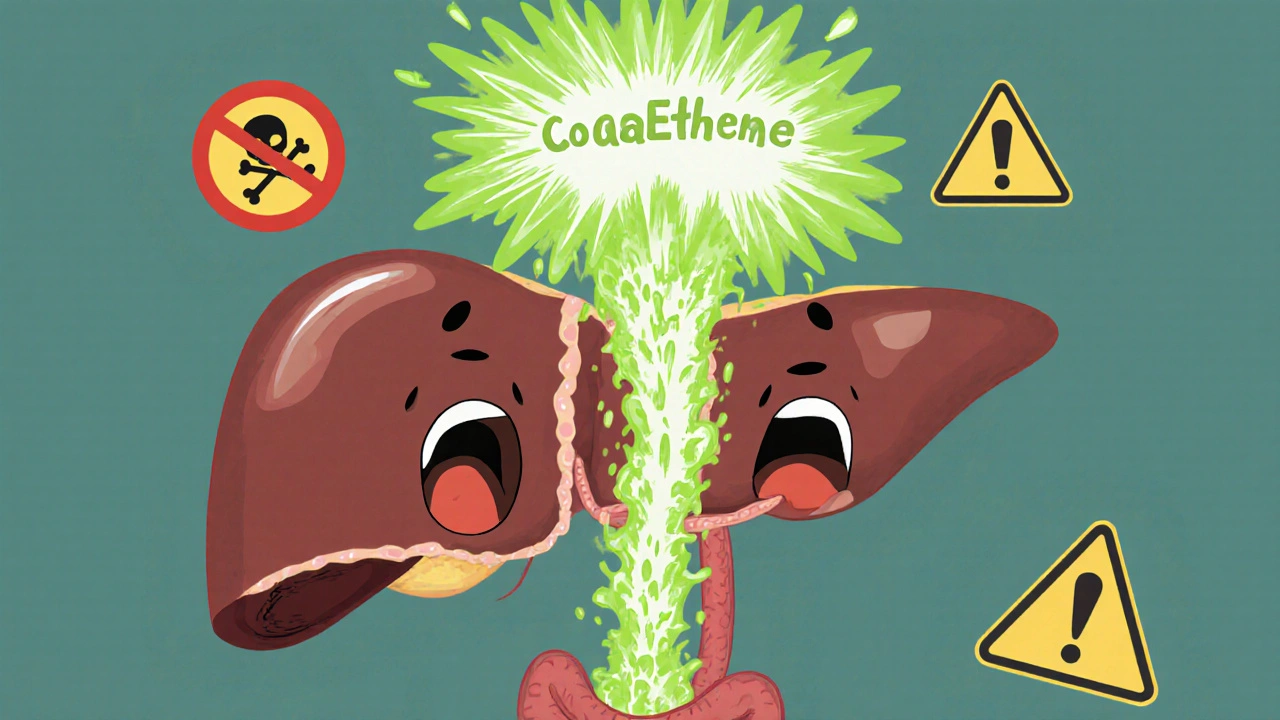
Alcohol and Cocaine: The Hidden Toxin Cocaethylene
Another deadly mix you might not know about: alcohol and cocaine. When these two are in your system at the same time, your liver creates a new chemical called cocaethylene. It’s more toxic than either drug alone. DrugAbuse.com reports cocaethylene increases the risk of sudden death by 25% compared to cocaine by itself.
Cocaethylene lasts longer in your body than cocaine, which tricks users into thinking they’re still high - so they take more. It also damages your liver. Studies show 65% of chronic users of this combo develop liver toxicity. Symptoms include extreme stomach pain, irregular heartbeat (over 140 bpm), seizures, and coma. Unlike the speedball, this mix doesn’t require heroin. Just a beer and a line of cocaine - and your body starts poisoning itself from the inside.
Antidepressants and Alcohol: A Silent Risk
Many people don’t realize their antidepressants can turn a drink into a danger zone. Duloxetine (Cymbalta) and venlafaxine (Effexor) are commonly prescribed for depression and anxiety. When mixed with alcohol, they increase liver stress. One 2018 study found alcohol with duloxetine raises liver toxicity risk by 40%. With venlafaxine, the threshold for a fatal alcohol overdose drops by 25%.
Even more concerning is the effect on mental health. Alcohol is a depressant. Antidepressants are meant to lift mood. When you mix them, you can feel worse - more anxious, more depressed, more confused. Some users report blackouts, memory loss, and intense emotional swings. It’s not just physical harm. It’s emotional chaos.
Buprenorphine and Alcohol: A Hidden Trap
If you’re using buprenorphine (Suboxone, Subutex) to treat opioid addiction, you might think you’re safe - as long as you’re not using heroin. But alcohol? That’s still dangerous. Buprenorphine lowers your blood pressure and slows your breathing. Alcohol does the same. Together, they can cause hypotension (blood pressure below 90/60), respiratory rates under 10 breaths per minute, and deep sedation that turns into coma.
The SA Health Department warns: "The more alcohol in the body, the less heroin needed to cause an overdose." The same applies to buprenorphine. Even a couple of drinks can push you into a life-threatening state. Many people in recovery think they’ve "graduated" from risk. But mixing alcohol with any opioid medication - even the ones used to treat addiction - is still a gamble with your life.
What You Can Do: Protect Yourself and Others
Knowing the risks isn’t enough. You need to act.
- Ask your doctor - every time you get a new prescription, ask: "Can I drink alcohol with this?" Don’t assume it’s safe just because it’s legal.
- Check your meds - use free online tools like WebMD’s Drug Interaction Checker or Medscape’s tool. They’re not perfect, but they flag the big red flags.
- Don’t mix street drugs - if you’re using cocaine, meth, or heroin, assume it’s laced with fentanyl. There’s no safe way to use these, especially with anything else.
- Carry naloxone - if you or someone you know uses opioids, keep naloxone (Narcan) on hand. It won’t help with alcohol or stimulants, but it can reverse opioid overdoses and save a life.
- Speak up - if you see someone mixing dangerous drugs, don’t ignore it. Talk to them. Call poison control (1-800-222-1222). It could be the difference between life and death.
Community programs that hand out naloxone and educate about polysubstance risks have cut overdose deaths by 22% in some areas. Awareness saves lives. You don’t need to be an expert to help. Just know the facts - and share them.
What’s Changing - And What’s Still Missing
There’s progress. The FDA now requires opioid labels to warn about alcohol and benzodiazepine interactions. AI-powered drug interaction screens are being added to electronic health records by 2025. These tools will help doctors catch dangerous combos before they’re prescribed.
But the real problem isn’t just prescriptions. It’s the lack of public awareness. Most people don’t know about cocaethylene. They don’t realize that taking two pills they’ve used before can become deadly when combined. The SAMHSA 2023 awareness campaign saw a 27% spike in poison control calls - proof that people are starting to ask questions. But we need more.
Every year, hundreds of thousands of people take medications without understanding how they interact. And every year, too many of them die because they didn’t know the risks. It doesn’t have to be this way. Knowledge is the first step. Action is the next.
Can mixing alcohol and painkillers really kill you?
Yes. Mixing alcohol with opioids like oxycodone, hydrocodone, or fentanyl can cause severe respiratory depression - your breathing slows so much that your brain stops getting oxygen. Even one or two drinks can be enough, especially if you’re not used to the medication. This combination is responsible for thousands of deaths each year.
Is it safe to take Xanax with a glass of wine?
No. Xanax (alprazolam) and alcohol are both CNS depressants. Together, they can cause extreme drowsiness, loss of coordination, memory blackouts, and respiratory failure. The risk of a fatal overdose increases by up to 300% compared to alcohol alone. Even small amounts can be dangerous.
What is cocaethylene and why is it dangerous?
Cocaethylene is a toxic chemical your liver produces when you mix cocaine and alcohol. It lasts longer in your body than cocaine alone and increases the risk of sudden death by 25%. It also damages your liver, raises your heart rate dangerously, and can trigger seizures or heart attacks. There’s no safe level of this combination.
Can antidepressants interact dangerously with alcohol?
Yes. Medications like Cymbalta and Effexor can increase liver damage when mixed with alcohol. They can also worsen depression, cause dizziness, and lower your tolerance for alcohol - meaning you can overdose on less than you think. Never assume your antidepressant is "safe" with drinks.
What should I do if I’ve been mixing drugs and now feel unwell?
Call poison control immediately at 1-800-222-1222. Don’t wait for symptoms to get worse. If someone is unconscious, not breathing, or having seizures, call 911 right away. If you have naloxone and suspect an opioid overdose, administer it. Time is critical - don’t hesitate.
Are there any safe drug combinations?
Some combinations are safe when used as directed by a doctor - but you must ask. Even common OTC meds like ibuprofen or acetaminophen can be risky with alcohol or certain prescriptions. The only way to know for sure is to check with your pharmacist or doctor. Never assume safety based on past experience.
Final Thought: It’s Not About Judging - It’s About Surviving
You don’t have to be an addict to be at risk. You don’t have to be using street drugs. You could be someone who takes their pain meds as prescribed and has a glass of wine with dinner. That’s how most of these deaths happen - quietly, without warning. The goal isn’t to scare you. It’s to give you the facts so you can make smarter choices. One conversation, one check of a drug interaction tool, one moment of hesitation before mixing substances - that’s all it takes to avoid tragedy.


mohit passi
November 25, 2025 AT 15:50Marissa Coratti
November 26, 2025 AT 20:51Micaela Yarman
November 27, 2025 AT 23:24Amanda Wong
November 29, 2025 AT 22:26james thomas
November 30, 2025 AT 19:31Deborah Williams
December 2, 2025 AT 18:33Kaushik Das
December 4, 2025 AT 16:20Asia Roveda
December 5, 2025 AT 00:21Aaron Whong
December 5, 2025 AT 19:54Sanjay Menon
December 6, 2025 AT 06:39Cynthia Springer
December 7, 2025 AT 03:38Rachel Whip
December 8, 2025 AT 18:04Ali Miller
December 9, 2025 AT 04:21JAY OKE
December 10, 2025 AT 08:17Joe bailey
December 10, 2025 AT 23:04Rachel Whip
December 11, 2025 AT 18:01