Statin Muscle Pain Checker
Symptom Assessment
Answer these questions to determine the likely cause of your muscle symptoms
When you start taking a statin to lower your cholesterol, you expect better heart health-not aching legs, weak arms, or constant fatigue. But for many people, muscle pain becomes the unexpected price of taking these life-saving drugs. Statin-induced muscle pain isn’t just a minor annoyance. It’s a real, measurable condition with different forms, some mild and others serious enough to require hospitalization. Understanding the difference between simple myalgia and dangerous myositis can make all the difference in how you manage your health.
What Exactly Is Statin-Induced Muscle Pain?
Statin-induced muscle pain, or statin myopathy, covers a range of muscle problems that happen after starting a statin. It’s not rare. Up to 30% of people taking statins report muscle discomfort. But not all muscle pain is the same. The most common form is myalgia: muscle aches, cramps, or stiffness without any rise in muscle enzymes. You feel sore, but your blood tests look normal. This type usually goes away within a week or two after stopping the statin.
Then there’s myositis-a more serious condition. This isn’t just soreness. It’s inflammation in the muscle tissue, confirmed by elevated levels of creatine kinase (CK) in the blood. CK levels above 10 times the normal range signal muscle damage. People with myositis often feel weak, especially when climbing stairs or lifting objects. Their muscles may feel tender to the touch. Unlike simple myalgia, myositis doesn’t just fade on its own. If left unchecked, it can lead to rhabdomyolysis, a rare but life-threatening breakdown of muscle tissue that can damage your kidneys.
And then there’s the rare but dangerous immune-mediated form: statin-associated autoimmune myopathy (SAAM). This isn’t just a side effect-it’s an autoimmune reaction. Your body starts attacking its own muscle tissue because it mistakes the HMG-CoA reductase enzyme (the same target of statins) as a threat. This form can strike even after you’ve stopped the statin. Symptoms get worse over months, not days. Muscle weakness spreads to your hips and shoulders. CK levels often soar past 2,000 IU/L (normal is 30-200). Many patients are misdiagnosed for over a year, told they have fibromyalgia or chronic fatigue. By the time they see a neuromuscular specialist, they’ve already lost significant strength.
Why Do Statins Cause Muscle Problems?
Statin drugs work by blocking HMG-CoA reductase, an enzyme your liver uses to make cholesterol. But that enzyme is also involved in producing other important molecules-ones your muscles need to function. When statins shut it down, they accidentally starve your muscles of key nutrients.
One of the biggest losses is coenzyme Q10 (CoQ10). This compound helps your muscle cells produce energy. Studies show that taking 40 mg of simvastatin daily can drop CoQ10 levels by 40%. Without enough CoQ10, your muscles run out of fuel. You feel tired, weak, and sore. That’s why some people try CoQ10 supplements-but the evidence is mixed. Only about 3 out of 7 clinical trials showed real improvement.
Another problem is protein breakdown. Statins crank up the activity of the ubiquitin-proteasome system-the body’s natural recycling program for old or damaged proteins. In muscle tissue, this system goes into overdrive, breaking down healthy proteins faster than they can be replaced. One study found this system becomes 300-400% more active in people on statins, especially if they do intense or unfamiliar exercise.
Then there’s calcium. Statins cause calcium to leak into muscle cells at abnormal levels. Too much calcium triggers enzymes that chew up muscle fibers. This is one reason why muscle damage can keep getting worse even after you stop the statin.
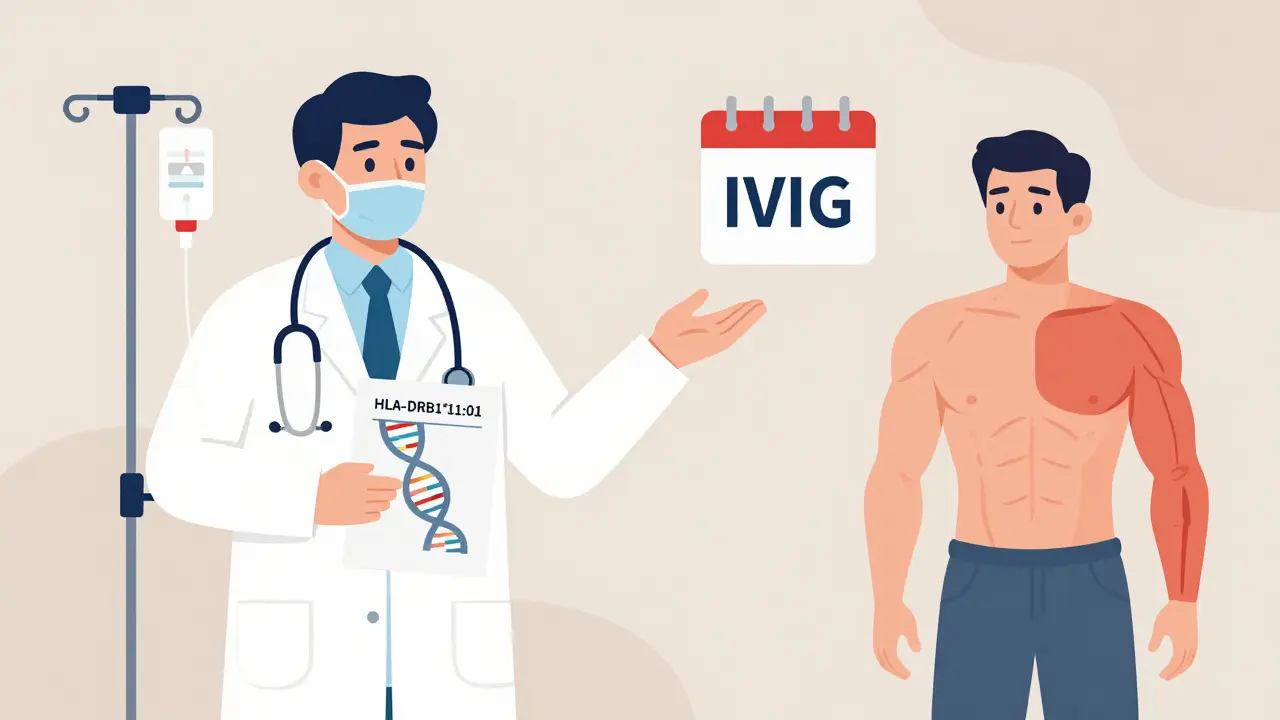
And for the autoimmune form-SAAM-genetics play a big role. People with a specific gene variant (HLA-DRB1*11:01) are far more likely to develop it. Statins actually cause muscle cells to make more of the HMG-CoA reductase enzyme. In genetically prone people, this overproduction tricks the immune system into attacking it. Once that starts, it doesn’t stop just because you quit the drug.
How Doctors Diagnose Statin Muscle Problems
Diagnosing statin myopathy isn’t just about asking if your muscles hurt. It’s a process of elimination. Your doctor will start by asking about your medication history. Are you on other drugs that interact with statins? Amiodarone, gemfibrozil, or even grapefruit juice can spike statin levels in your blood and make muscle damage worse.
A simple blood test checks your creatine kinase (CK) levels. Normal is 30-200 IU/L. If your CK is above 10 times that, it’s a red flag. But here’s the catch: some people with severe muscle pain have normal CK levels. That’s why muscle biopsy is still the gold standard for diagnosing SAAM. A biopsy shows muscle fibers dying with almost no inflammation-exactly what you’d expect from an autoimmune attack.
Other tools help too. Electromyography (EMG) can detect abnormal electrical patterns in muscles. Muscle MRI shows swelling in the thighs or hips. And now, a new blood test is emerging: a panel of microRNAs (miR-206 and miR-133a) that can distinguish autoimmune myopathy from regular statin pain with 89% accuracy.
Don’t forget thyroid and vitamin D. Low thyroid function and vitamin D deficiency can also cause muscle pain. If those are low, fixing them might clear up the symptoms-no statin change needed.
What to Do If You Have Muscle Pain on Statins
If you notice new muscle pain after starting a statin, don’t ignore it. But don’t panic either. Most cases are mild. Here’s what to do:
- Stop the statin and contact your doctor. Don’t wait to see if it gets better.
- Get a CK test. If it’s normal, you likely have myalgia. If it’s high, you need further testing.
- Rule out other causes: check thyroid and vitamin D levels.
- If symptoms persist beyond 3 months, ask for anti-HMGCR antibody testing.
If you’re diagnosed with SAAM, you’ll need a specialist. Treatment isn’t just stopping the statin. You’ll likely need immunosuppressants-prednisone, methotrexate, or mycophenolate. In severe cases, IVIG (intravenous immunoglobulin) or the newer drug ravulizumab may be used. The sooner you start treatment, the better your chances of recovery. Patients treated within 6 months of symptoms start have a 65% chance of full recovery. If you wait over a year, that drops to 28%.
For those with mild myalgia who still need cholesterol control, alternatives exist. Switching to a different statin helps. Rosuvastatin is often better tolerated than simvastatin. Some people do well on lower doses taken every other day. Others switch to non-statin options like ezetimibe or PCSK9 inhibitors, which don’t cause muscle issues.
Who’s at Higher Risk?
Not everyone is equally likely to get statin muscle pain. Certain factors raise your risk:
- Age: People over 65 are more sensitive.
- Gender: Women report muscle pain more often than men.
- Genetics: The SLCO1B1 gene variant rs4149056 doubles your risk of simvastatin myopathy.
- Race: African Americans have nearly twice the risk of Caucasians.
- Medications: Drugs like amiodarone, cyclosporine, or fibrates increase statin levels.
- Health status: Kidney disease, hypothyroidism, and low vitamin D make muscle damage more likely.
And here’s something surprising: statin type matters. Atorvastatin (Lipitor) shows up in over 40% of reported muscle pain cases-even though it’s not the most prescribed statin. Why? It’s widely used, and it’s metabolized in a way that can build up in muscle tissue.
The Bigger Picture: Balancing Risk and Benefit
Yes, statins can cause muscle pain. But they also prevent heart attacks and strokes. For someone with a history of heart disease or very high cholesterol, the benefits usually outweigh the risks. The problem isn’t statins themselves-it’s how we handle side effects.
Too many people quit statins because of muscle pain, not realizing they’ve increased their 10-year risk of a heart event by 25%. That’s why finding the right solution matters more than just stopping the drug. A good doctor won’t just say, “Stop the statin.” They’ll help you find a way to keep your heart protected without wrecking your muscles.
Future tools will make this easier. Pharmacogenomic testing-checking your genes before prescribing statins-is already being studied. Within five years, doctors may use genetic scores to pick the safest statin for you before you even start. Until then, listen to your body. Track your symptoms. Ask questions. And don’t let fear stop you from getting the care you need.
Can statin muscle pain go away on its own?
Yes, in most cases. If you have simple myalgia-muscle aches without elevated creatine kinase-symptoms usually fade within 1 to 2 weeks after stopping the statin. But if your pain persists beyond 3 months, gets worse, or includes weakness, it could be something more serious like immune-mediated myopathy. That won’t go away on its own and needs medical treatment.
Does CoQ10 help with statin muscle pain?
Some people feel better taking CoQ10 supplements, but the science isn’t strong. Studies show mixed results: only about 3 out of 7 trials found a meaningful reduction in muscle pain. It may help a little if your CoQ10 levels are low, but it won’t fix immune-mediated myopathy. Don’t rely on it as a cure.
Can I switch to a different statin if I have muscle pain?
Yes, many people tolerate a switch well. Rosuvastatin and pravastatin are often better tolerated than simvastatin or atorvastatin because they’re processed differently in the body. A 2021 study found 73% of people who couldn’t take simvastatin could handle rosuvastatin after switching. Lower doses or taking the statin every other day can also help.
How do I know if I have the autoimmune form (SAAM)?
SAAM shows up as progressive muscle weakness that gets worse over months, even after stopping the statin. Your CK levels are usually very high-over 2,000 IU/L. You might also have trouble raising your arms or standing from a chair. A blood test for anti-HMGCR antibodies and a muscle biopsy are needed to confirm it. If you’ve had symptoms for over 3 months, ask your doctor about these tests.
Is muscle pain from statins a sign of heart problems?
No, muscle pain itself isn’t a sign of heart problems. But stopping your statin because of muscle pain can increase your risk of heart attack or stroke. The pain is a side effect of the drug, not a warning from your heart. The goal is to manage the muscle issue so you can keep taking a cholesterol-lowering medication that protects your heart.
Can exercise make statin muscle pain worse?
Yes, especially intense or unfamiliar exercise like heavy lifting or long-distance running. Statins already increase muscle protein breakdown. Adding extreme physical stress can push your muscles past their limit. Stick to moderate, consistent activity like walking or swimming. Avoid sudden spikes in intensity.


Amanda Eichstaedt
January 11, 2026 AT 19:32My mom was on simvastatin for years and started having leg cramps so bad she couldn’t sleep. Doctor said it was just aging-until her CK hit 4,200. Turned out SAAM. Took her six months to get diagnosed. Now she’s on IVIG and can walk again. Don’t let anyone tell you it’s ‘just soreness.’
Daniel Pate
January 12, 2026 AT 18:54It’s wild how we treat statins like magic pills without acknowledging they’re basically molecular sledgehammers. Blocking HMG-CoA reductase doesn’t just lower cholesterol-it disrupts the entire mevalonate pathway. CoQ10 depletion, calcium leaks, protein degradation-it’s a cascade. We’re treating symptoms while ignoring the systemic sabotage.
And yet, the pharmaceutical industry pushes these drugs like they’re vitamin supplements. The real scandal isn’t the side effects-it’s that we don’t screen for HLA-DRB1*11:01 or SLCO1B1 before prescribing. This isn’t medicine. It’s genetic roulette.
Alex Fortwengler
January 13, 2026 AT 03:05Big Pharma knows this is happening and still pushes statins because they make billions. CoQ10 supplements? A joke. They don’t want you to fix it-they want you to keep taking the drug and buy more pills for the side effects. And don’t get me started on how they bury the SAAM data. It’s all about profit, not patients.
Bryan Wolfe
January 14, 2026 AT 09:08I’ve seen this too many times-people panic and quit statins cold turkey because their legs hurt, then end up in the ER with a heart attack because they thought muscle pain = ‘stop everything.’ The key isn’t quitting-it’s working with your doc to find a version that works. Rosuvastatin at 5mg every other day? That’s my sweet spot. No pain, LDL under 70. It’s not one-size-fits-all.
Jennifer Phelps
January 15, 2026 AT 02:52So if CK is normal but muscles hurt is it still statin related or just coincidence
Amanda Eichstaedt
January 15, 2026 AT 10:33Exactly. Normal CK doesn’t mean it’s not real. I had a friend with SAAM whose CK was barely elevated-but she couldn’t lift a coffee cup. Biopsy showed fiber necrosis. That’s the trap. Doctors rely too much on labs and not enough on patient experience.
Katherine Carlock
January 16, 2026 AT 20:18I switched from atorvastatin to pravastatin after 3 months of leg pain and it was like a miracle. No more soreness, no weakness. My doctor said it’s because pravastatin doesn’t cross into muscle tissue as easily. So yeah, not all statins are the same. Try a different one before giving up.
Sona Chandra
January 17, 2026 AT 09:51My cousin’s husband died from rhabdomyolysis after ignoring his pain for months. He was told it was ‘just aging’ and ‘you’re too active.’ Now he’s in a grave and they still won’t admit statins were the trigger. This is a silent killer and nobody talks about it enough.
Lawrence Jung
January 18, 2026 AT 01:36People think muscle pain is bad but they don’t realize heart disease kills 100x more. You want to live longer? Take the statin. Your muscles will adapt. If you can’t tolerate it then maybe you’re just weak
Daniel Pate
January 19, 2026 AT 23:09That’s the exact mindset that gets people killed. ‘Just take it and adapt’ ignores the fact that muscle damage isn’t just discomfort-it’s irreversible cell death. And for SAAM? There’s no adaptation. It’s a runaway autoimmune train. You don’t ‘adapt’ to your immune system eating your muscles. You get treated. Or you lose function. Forever.
And no, heart disease doesn’t kill 100x more than statin myopathy because we catch most of it early. But we don’t catch SAAM early because doctors don’t know to look for it. That’s the real epidemic: ignorance, not statins.