Arrhythmias: What to watch, what to do
If your heart skips, races, or feels like it's fluttering, that can be an arrhythmia. You don't need medical jargon to understand it. An arrhythmia means the heart's electrical signals are off rhythm. Some are harmless. Others need fast treatment. This page helps you spot the difference and take the next step.
Common types and symptoms
Atrial fibrillation (AF) is the most talked-about arrhythmia. It feels like a fast, irregular heartbeat and can cause shortness of breath, lightheadedness, or fatigue. Premature ventricular contractions (PVCs) are extra beats you might feel as a flip or skip. Supraventricular tachycardia (SVT) starts suddenly and makes your heart race. Bradycardia means a slow heart rate and can cause fainting or tiredness.
Warning signs that need quick care: chest pain, fainting, severe shortness of breath, or a very fast pulse over 150–180 bpm. Mild palpitations without other symptoms are common and often harmless, but check with your doctor if they happen often or feel different than usual.
Tests, treatments, and everyday steps
Doctors use ECGs, Holter monitors, event recorders, and sometimes an implantable loop recorder to catch rhythm problems. Blood tests and an echocardiogram help find causes like thyroid problems or structural heart disease. Treatment depends on type and risk. For AF, options include rate control (beta-blockers, calcium channel blockers), rhythm control (antiarrhythmic drugs), and blood thinners to reduce stroke risk.
Procedures matter too. Catheter ablation targets the faulty tissue causing AF or SVT and can stop symptoms for many people. Pacemakers treat slow rhythms. In emergencies, cardioversion resets the heart with electricity. Your doctor will weigh benefits and risks with you, based on age, other health issues, and lifestyle.
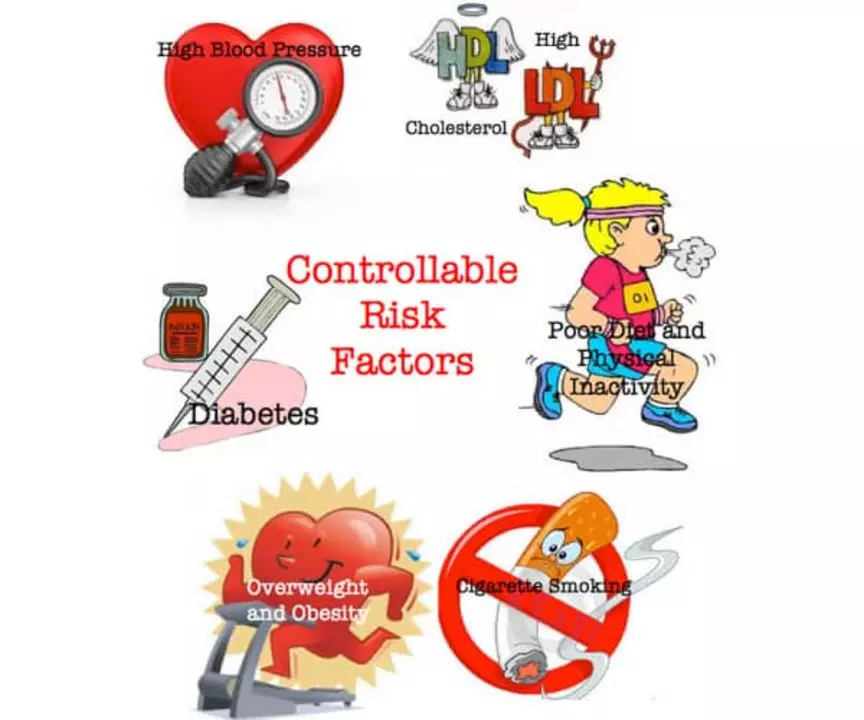
Small daily changes help a lot. Cut back on caffeine and excess alcohol if palpitations bother you. Keep hydrated, manage stress, and sleep well. If you smoke or have untreated high blood pressure, get help to quit or control it. These steps lower your chance of serious arrhythmias over time.
When you get a diagnosis, ask clear questions: What type do I have? Do I need medication or a procedure? What are the risks of stroke? How will this affect work, driving, or exercise? Bring a family member to appointments if you can; two heads remember more details.
If you ever faint, have crushing chest pain, or feel very short of breath, call emergency services right away. For ongoing symptoms, start with your primary doctor or a cardiologist who treats arrhythmias. Early action often means simpler, safer treatment and fewer surprises down the road.
Want quick tools? Track your pulse for 30 seconds when resting. Note frequency, triggers, and how long episodes last. Share that info with your doctor — it speeds up diagnosis and gets you the right care sooner.
The Connection between Arrhythmias and Stroke
As a blogger, I've recently come across an interesting topic that I'd like to share with you - the connection between arrhythmias and stroke. Arrhythmias are irregular heartbeats, which can disrupt the normal flow of blood and potentially lead to blood clots. These clots can then travel to the brain and cause a stroke, which can be life-threatening. It's crucial to be aware of this connection and monitor any heart-related issues, as managing arrhythmias can help prevent strokes. Remember, staying informed and taking care of your heart can go a long way in ensuring your overall health.
- May 11 2023
- Tony Newman
- 17 Comments
