Understanding the Basics: Arrhythmias and Stroke
Before we dive into the connection between arrhythmias and stroke, it's essential to understand what these terms mean. Arrhythmia is a term used to describe irregular heart rhythms. These can be caused by various factors, such as electrical issues in the heart, damage to the heart muscle, or underlying health conditions. On the other hand, a stroke occurs when blood flow to a part of the brain is interrupted, leading to brain tissue damage and potential long-term complications. In this section, we'll break down the basics of arrhythmias and stroke, and how the two are connected.
The Role of Atrial Fibrillation in Stroke Risk
Atrial fibrillation (AFib) is the most common type of arrhythmia linked to an increased risk of stroke. AFib causes the upper chambers of the heart (the atria) to beat irregularly and often rapidly, leading to poor blood flow and the potential for blood clots to form. These clots can then travel through the bloodstream to the brain, resulting in a stroke. In fact, people with AFib are five times more likely to experience a stroke than those without the condition. In this section, we'll explore the role of atrial fibrillation in stroke risk and discuss prevention strategies.
Other Arrhythmias that Contribute to Stroke Risk
Although atrial fibrillation is the most common arrhythmia associated with stroke, other types of arrhythmias can also contribute to stroke risk. For example, ventricular tachycardia—an abnormally fast heart rate originating in the lower chambers of the heart (the ventricles)—can lead to decreased blood flow to the brain, increasing the risk of stroke. Additionally, certain types of heart block—a condition in which electrical signals between the atria and ventricles are disrupted—can also increase stroke risk. In this section, we'll discuss other arrhythmias that contribute to stroke risk and the importance of proper diagnosis and treatment.
Signs and Symptoms of Arrhythmias and Stroke
Recognizing the signs and symptoms of arrhythmias and stroke can be life-saving. Common symptoms of arrhythmias include palpitations (a feeling of skipped or extra heartbeats), shortness of breath, dizziness, lightheadedness, and chest discomfort. On the other hand, stroke symptoms usually come on suddenly and may include sudden numbness or weakness on one side of the body, sudden confusion or trouble speaking, sudden vision problems, sudden trouble walking or loss of balance, and a sudden severe headache with no known cause. In this section, we'll dive deeper into the signs and symptoms of arrhythmias and stroke, and discuss the importance of seeking immediate medical attention if you suspect a stroke.
Preventing Stroke in Individuals with Arrhythmias
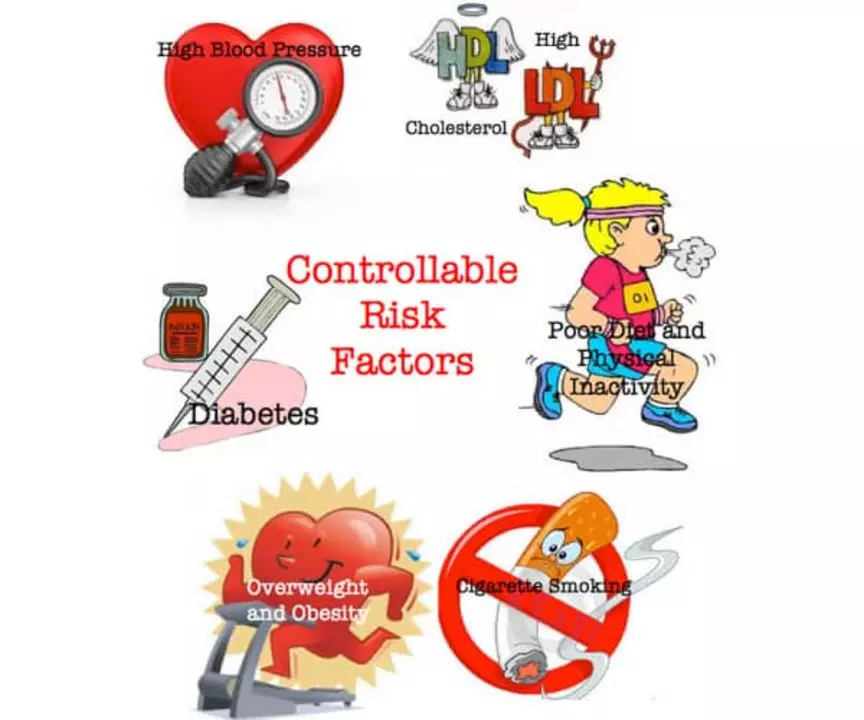
Fortunately, there are steps that individuals with arrhythmias can take to reduce their risk of stroke. These may include lifestyle changes, such as adopting a heart-healthy diet, engaging in regular physical activity, quitting smoking, and reducing stress. In some cases, medications may be prescribed to help control heart rate, prevent blood clots, and manage other risk factors for stroke. In more severe cases, medical procedures or surgeries may be recommended to treat the underlying cause of the arrhythmia. In this section, we will discuss various prevention strategies for individuals with arrhythmias, and how these measures can substantially reduce stroke risk.
Life After a Stroke: Recovery and Rehabilitation
For those who have experienced a stroke, the recovery process can be challenging and often involves a multidisciplinary approach to rehabilitation. This may include physical therapy to help regain strength and coordination, occupational therapy to assist with daily tasks, speech therapy to address communication and swallowing difficulties, and psychological support to manage the emotional impact of stroke. Additionally, ongoing management of arrhythmias and other stroke risk factors is crucial to prevent a recurrent stroke. In this final section, we'll explore the journey of recovery and rehabilitation after a stroke, and the importance of ongoing care and support.

Mary Akerstrom
May 11, 2023 AT 20:14Great overview thanks for sharing.
Delilah Allen
May 12, 2023 AT 04:53The connection between heart rhythm disorders and cerebrovascular events is not just a theoretical concept, it is a stark clinical reality; when atrial fibrillation goes unchecked, clots can form with alarming speed, and those emboli may slam into cerebral vessels, causing immediate damage. Moreover, studies consistently show that patients with AFib have a dramatically higher incidence of ischemic stroke, sometimes five times greater than the general population; this statistic alone should provoke urgent action. Yet, many clinicians still underestimate the silent progression of arrhythmias, ignoring subtle palpitations or occasional dizziness, which are often the only early warnings. The pathophysiology is clear: irregular atrial contractions promote stasis of blood, leading to thrombus formation, and once dislodged, these clots travel to the brain, blocking critical arteries. Prevention strategies must therefore target both rhythm control and anticoagulation, a dual approach that has proven effective in reducing stroke rates. Lifestyle modifications, such as reducing sodium intake, quitting smoking, and engaging in regular aerobic exercise, can lower the burden of arrhythmias, but they are insufficient without medical therapy for high‑risk individuals. Anticoagulants, whether warfarin or newer direct oral agents, dramatically cut the odds of stroke, yet patient adherence remains a stubborn obstacle. Education is paramount, and patients need clear guidance on the signs of both arrhythmias and stroke, because time is brain. In emergency settings, rapid identification of irregular heartbeats can expedite stroke work‑ups, potentially saving lives. The healthcare system must also streamline referrals to electrophysiology specialists, ensuring timely ablation procedures when appropriate. Finally, ongoing research into personalized risk scores promises to refine our ability to predict which patients will benefit most from aggressive intervention, moving us closer to a future where stroke secondary to arrhythmia is a rarity. All of these measures, combined with vigilant monitoring, create a comprehensive defense against a devastating outcome, and they must be embraced without hesitation.
Nancy Lee Bush
May 12, 2023 AT 13:33Wow, this article really dives deep into the heart‑brain link, & it’s super helpful! :) The way atrial fibrillation can spawn clots, then zip straight to the brain, is both fascinating and terrifying; it underscores why early detection matters. Also, the lifestyle tips-like cutting down on salty snacks and staying active-are spot‑on, and they resonate with anyone wanting to keep their ticker healthy. The section on anticoagulants really clarifies the pros and cons, making the decision process less blurry. Keep up the great work, and thanks for breaking it down so clearly! :D
Dan Worona
May 13, 2023 AT 01:00Everyone’s talking about atrial fibrillation and strokes like it’s just a medical fact, but have you considered who’s really benefitting from this narrative? The pharmaceutical giants push anticoagulants as the ultimate solution, yet they downplay the long‑term side effects, creating a dependency loop that fuels their profits. Meanwhile, the data on hidden arrhythmia triggers-like electromagnetic fields from 5G towers-is conveniently omitted from mainstream discussions. It’s no coincidence that the same labs that manufacture these drugs also fund the research that validates their safety. We need to question the agenda and demand transparency, because the truth is being obscured by a web of interests.
Chuck Bradshaw
May 13, 2023 AT 12:26Let me set the record straight: the mechanisms linking arrhythmias to cerebral ischemia have been elucidated for decades, and the therapeutic protocols are well‑established. Any suggestion that current guidelines are inadequate reflects a misunderstanding of the underlying electrophysiology. Anticoagulation therapy, when monitored correctly, reduces stroke risk by up to 70%, and this is supported by robust randomized trials. Therefore, focusing on peripheral lifestyle tweaks without emphasizing evidence‑based medication is misguided.
Howard Mcintosh
May 13, 2023 AT 23:53Hey Chuck, u r right about the data but dont forget many ppl cant afford those meds or dont have proper follow‑up. its realy hard for them to keep up with blood tests. maybe we should talk more about community programs that can help with those barriers?
Jeremy Laporte
May 14, 2023 AT 11:20Yo Chuck, love the stats but let’s keep it real – not everyone’s gonna get a fancy anticoag. I think we need some down‑to‑earth tips, like free local health fairs or apps that remind folks to check their pulse. those can really make a diff.
Andy Lombardozzi
May 14, 2023 AT 22:46The precision of contemporary anticoagulation protocols is noteworthy; nevertheless, adherence challenges persist, underscoring the need for patient‑centred education initiatives.
Joshua Ardoin
May 15, 2023 AT 10:13Yo, this is 🔥! The brain‑heart connection is like a wild dance, and we’ve gotta keep the rhythm smooth. 💃🧠💓 If we skip the beat, you know the fallout-stroke city. Let’s spread the word, stay active, and keep those vibes good! 🌟😊
Glenn Gould
May 15, 2023 AT 21:40Yo Joshua, i feel u! staying active is key but a lot of peopple don't even know they have arrhythmia. we need more free checks in communities, maybe at local gyms or churches. also, big shout out to u for keepin it real!
Poonam Sharma
May 16, 2023 AT 09:06THIS IS A CALL TO ACTION FOR EVERY PATRIOT! The heart‑brain nexus is a battlefield, and we cannot let Western pharma dictate the rules. We must embrace indigenous health wisdom, reject the chemical leeches, and fortify our vessels with natural, home‑grown strategies. ONLY BY RECLAIMING OUR BODY’S SOVEREIGNTY CAN WE PREVENT THE SNEAKY STROKE ASSAULT! THIS IS NOT A DISCUSSION, THIS IS A MISSION!
Mita Son
May 16, 2023 AT 20:33While your passion is palpable, the scientific literature indicates that anticoagulation remains the gold standard for AFib‑related stroke prevention; alternative approaches lack rigorous validation. Nonetheless, integrating diet and exercise can complement, not replace, evidence‑based therapy.
ariel javier
May 17, 2023 AT 08:00The article provides a thorough overview; however, it fails to sufficiently address the nuances of risk stratification in patients with co‑morbid conditions, which is a critical oversight.
Bryan L
May 17, 2023 AT 19:26I appreciate the thoroughness of the analysis; it’s essential to remember that behind each statistic is a person’s life, and compassionate care can make a world of difference. 😊
joseph rozwood
May 18, 2023 AT 06:53While the content is ostensibly comprehensive, the prose oscillates between redundant verbosity and underwhelming brevity, betraying a lack of editorial discipline; moreover, the citation density suggests an overreliance on secondary sources, undermining the piece’s scholarly gravitas.
Richard Walker
May 18, 2023 AT 18:20It’s fair to critique the style, yet the core information remains valuable, especially for readers seeking a concise synthesis of arrhythmia‑related stroke risk.
Julien Martin
May 19, 2023 AT 05:46Indeed, the article’s substance is solid; integrating jargon‑heavy terminology like “thromboembolic cascade” can enhance precision, but balancing it with accessible language ensures broader comprehension.