Autoimmune: Practical steps to spot flares and manage life
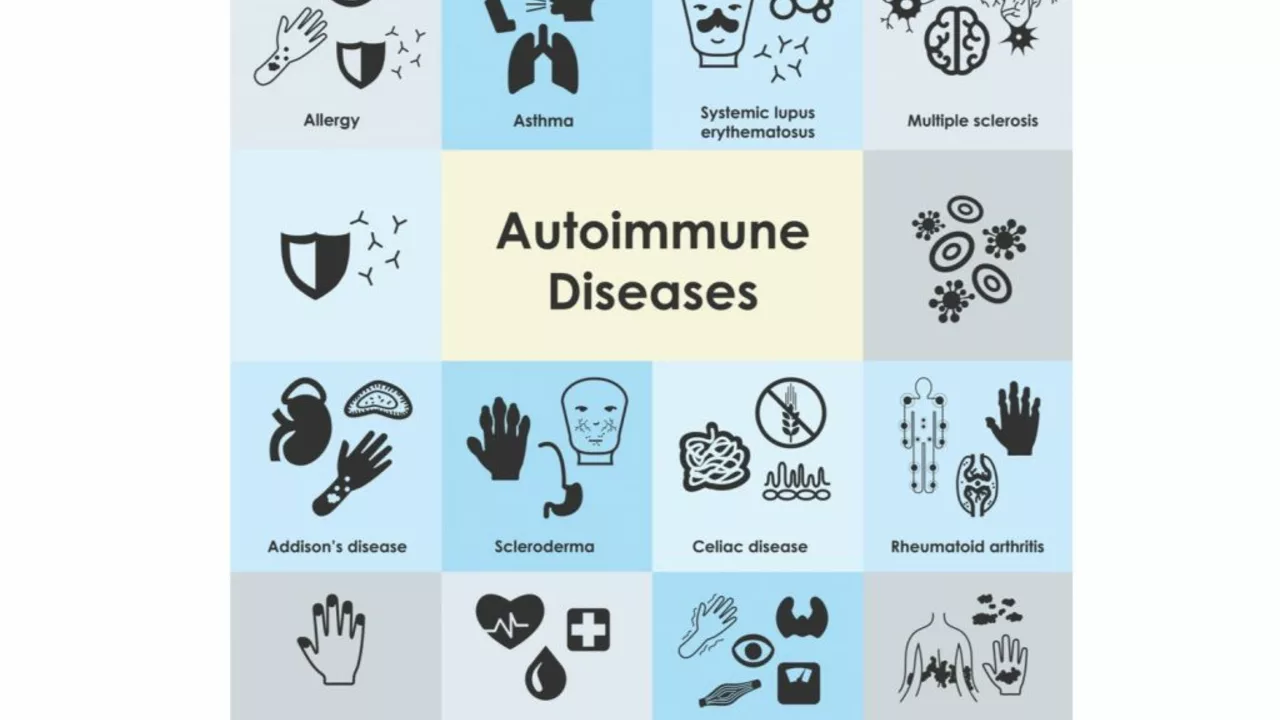
Autoimmune conditions happen when your immune system mistakenly attacks healthy tissue. That can sound scary, but knowing the common signs and what to do next makes a big difference. Want fewer surprise flares and clearer conversations with your doctor? Start here.
Common signs and quick checks
Symptoms vary by disease, but some red flags show up a lot: unexplained fatigue, joint pain or swelling, skin rashes, persistent low-grade fever, numbness or tingling, and odd digestive problems. If a symptom sticks around for weeks or shows up in multiple parts of your body, write it down. Track when it worsens, what you were doing, and any triggers like stress, food, or weather changes. That timeline helps doctors make sense of patterns.
Doctors use basic tests to look for autoimmune activity: ANA (antinuclear antibody), ESR and CRP (inflammation markers), and disease-specific antibodies for conditions like thyroid disease or celiac. Imaging or a biopsy can be needed sometimes. If your primary care doc seems unsure, ask for a referral to a rheumatologist, dermatologist, or neurologist depending on symptoms.
Treatment approaches that actually help
Treatment depends on the condition and how active it is. Short-term steroids can calm a flare quickly. For long-term control, doctors often use disease-modifying drugs (DMARDs) or biologics that target parts of the immune system. Newer small-molecule medicines also help some people. Always ask what each option does, how long it takes to work, and what side effects to watch for.
Beyond prescriptions, daily habits matter. Aim for consistent sleep, gentle movement (walking, stretching, low-impact strength), and a simple anti-inflammatory eating pattern—more veggies, fatty fish, whole grains, fewer ultra-processed foods. Vitamin D and omega-3 supplements help many people, but check levels and talk to your clinician before starting anything new.
Because immune-suppressing meds raise infection risk, stay up to date on vaccines your doctor recommends and speak up fast if you get a fever. Also, plan for mental health: chronic disease wears on mood and motivation. Support groups, short-term therapy, or a trusted online community can make day-to-day easier.
Medication access is another real issue. If you look at online pharmacies, verify accreditation and require a prescription. Cheap sites without credentials can sell counterfeit or unsafe drugs. Our site covers safer ways to source meds online and alternatives if certain drugs aren’t available.
Practical tips to use tomorrow: keep a symptom log, carry a list of current meds and allergies, schedule regular check-ins with your specialist, and set one small habit (like a 10-minute evening walk) that you can keep doing. Small consistent steps add up.
If you want articles on diet approaches, steroid alternatives, or how specific drugs work, check our related guides for clearer, usable steps. And when in doubt—ask your doctor a direct question and bring your notes. That short conversation often changes the next few months for the better.
Lupus and Allergies: What's the Connection?
As a lupus patient, I've always wondered about the connection between lupus and allergies. It turns out that lupus, an autoimmune disease, can cause an overactive immune system that may lead to increased allergies. This means that our bodies might react more strongly to allergens, making us more prone to allergic reactions. Moreover, some lupus medications can also cause or worsen allergies. It's essential for those with lupus to be aware of this connection and take necessary precautions to manage their allergies effectively.
- June 18 2023
- Tony Newman
- 15 Comments
