Cardiac Drug Safety: What You Need to Know About Heart Medications and Risks
When you're taking medicine for your heart, cardiac drug safety, the practice of using heart medications in a way that minimizes harm while maximizing benefit. Also known as heart drug safety, it's not just about remembering to take your pills—it's about understanding what else might be in your system that could turn a safe dose into a life-threatening event. Millions of people rely on drugs like beta blockers, ACE inhibitors, or blood thinners every day. But for every person who benefits, someone else ends up in the ER because they didn’t know their supplement, their coffee, or their painkiller was mixing dangerously with their heart medication.
One of the biggest risks isn’t the drug itself—it’s the dangerous drug interactions, when two or more medications or substances combine in a way that causes unexpected, harmful effects. For example, taking aspirin with warfarin might seem harmless, but together they can turn a minor cut into uncontrolled bleeding. Even something as simple as grapefruit juice can block how your body breaks down statins, causing muscle damage. And then there’s the silent danger: anticoagulants, medications that prevent blood clots but require careful monitoring to avoid bleeding. If you’re on one of these, a fall, a dental procedure, or even a new herbal supplement like ginkgo biloba can push you into serious trouble.
blood thinners, a category that includes both older drugs like warfarin and newer ones like DOACs are especially tricky because their effects aren’t always obvious. You won’t feel a clot forming, and you won’t always feel the bleeding either—until it’s too late. That’s why knowing your INR levels, understanding your doctor’s dosing instructions, and telling every provider you see—including your dentist—what you’re taking isn’t optional. It’s survival.
Cardiac drug safety also means recognizing the difference between a side effect and a real allergic reaction. Feeling tired on bisoprolol? That’s common. Swelling your throat after taking a new pill? That’s an emergency. Mislabeling one as the other can lead to doctors avoiding drugs you actually need. And with so many people on multiple medications—especially older adults—the risk of polypharmacy grows. One pill might be fine. Two might be okay. But five? That’s when things start to unravel.
What you’ll find below are real, practical guides written by people who’ve seen the consequences of ignoring these risks. From how to avoid deadly combinations like opioids and benzodiazepines, to why your evening primrose oil might be triggering seizures when you’re on antipsychotics, to how the FDA is changing how drug information is presented to patients—this isn’t theory. These are the stories behind the warnings. The mistakes people make. The fixes that work. You don’t need to be a doctor to protect yourself. You just need to know what to ask, what to watch for, and when to speak up.
Amiodarone, Digoxin, and Warfarin: The Dangerous Drug Triad You Can't Ignore
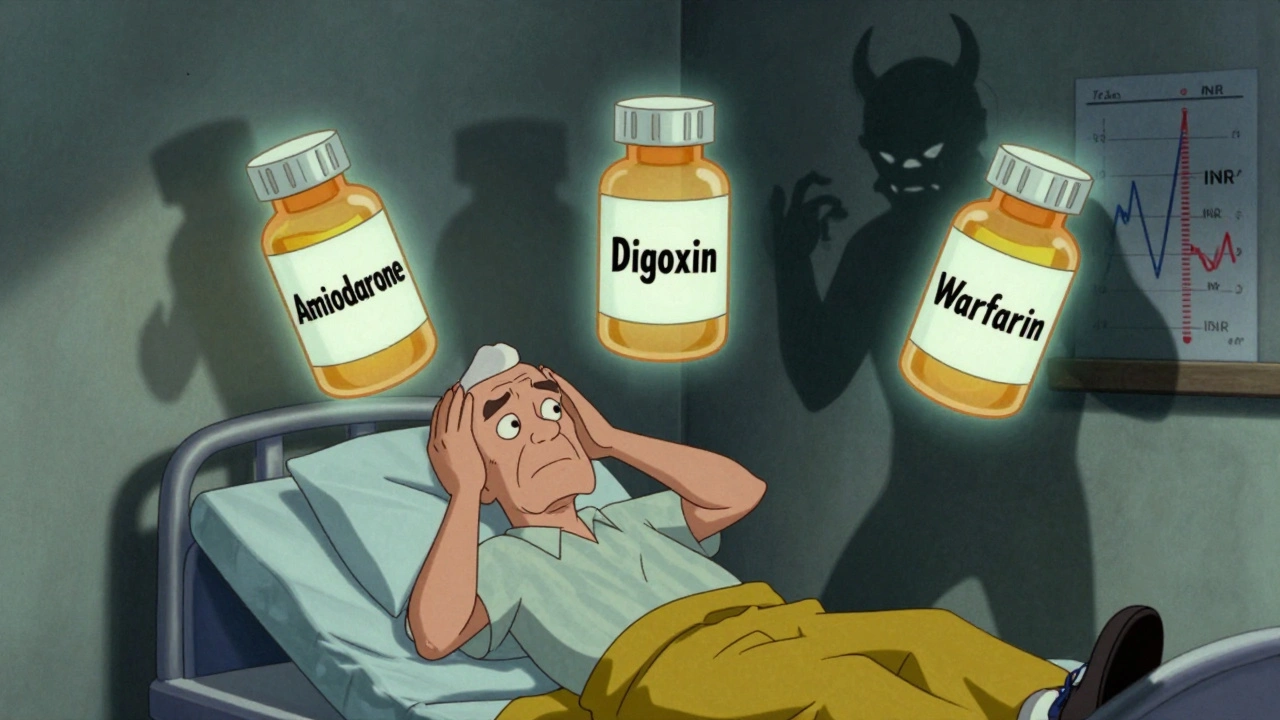
Amiodarone, digoxin, and warfarin together create a deadly drug interaction that can cause toxic digoxin levels and life-threatening bleeding. Learn how to spot the signs, adjust doses safely, and protect yourself or a loved one.
- December 4 2025
- Tony Newman
- 8 Comments
