Epidural Hematoma: Causes, Risks, and What You Need to Know
When you hit your head hard enough, something dangerous can happen inside your skull: an epidural hematoma, a collection of blood between the skull and the outer covering of the brain. Also known as extradural hematoma, it’s not a slow leak—it’s a fast-spreading pressure build-up that can crush brain tissue if not treated right away. This isn’t just a bruise. It’s a neurological emergency that often follows a sharp blow to the head, like from a fall, car crash, or sports injury. The bleeding usually comes from a torn artery, most commonly the middle meningeal artery, right under the skull’s thinnest part—right above the temple.
What makes an epidural hematoma, a collection of blood between the skull and the outer covering of the brain so dangerous is how quickly it can turn from a minor bump to life-threatening. Many people feel fine right after the injury, then suddenly get worse—confused, drowsy, or even unconscious. That’s the classic "lucid interval"—a deceptive calm before the storm. Kids and young adults are more at risk because their skulls are still flexible and the arteries are tightly anchored, making them easier to tear. Older adults? They’re more likely to have a different kind of bleed, called a subdural hematoma, because their brain has shrunk slightly and veins stretch more easily.
The key to surviving an epidural hematoma, a collection of blood between the skull and the outer covering of the brain is speed. A CT scan is the go-to test—it shows the blood as a bright, lens-shaped mass right under the skull. Surgery isn’t always needed, but if the clot is big or pressure is rising fast, doctors drill a hole (a burr hole) to drain it. Delay even an hour, and brain damage or death becomes much more likely. That’s why anyone with a serious head injury should go to the ER, even if they seem okay at first.
You won’t find this in every head injury guide, but here’s what matters: traumatic brain injury, damage to the brain caused by external force doesn’t always mean you’ll lose consciousness. Sometimes, the only sign is a headache that won’t quit, nausea, or one pupil larger than the other. And while intracranial bleeding, any bleeding inside the skull can come from veins or arteries, epidural hematomas are uniquely tied to trauma—never from a blood thinner or a stroke. That’s why knowing the difference matters.
What you’ll find in the posts below isn’t just theory. It’s real-world advice from people who’ve had to navigate medication risks after brain trauma, manage side effects from drugs used in recovery, or figure out if their symptoms are from the injury itself or the pills they’re taking. You’ll see how deprescribing, drug interactions, and lifestyle changes play into healing—not just the injury, but the whole system around it. These aren’t generic tips. They’re the kind of insights you wish you’d had before walking into a hospital with a head injury and a bag full of prescriptions.
Epidural and Spinal Procedures on Anticoagulants: What You Need to Know About Hematoma Risks
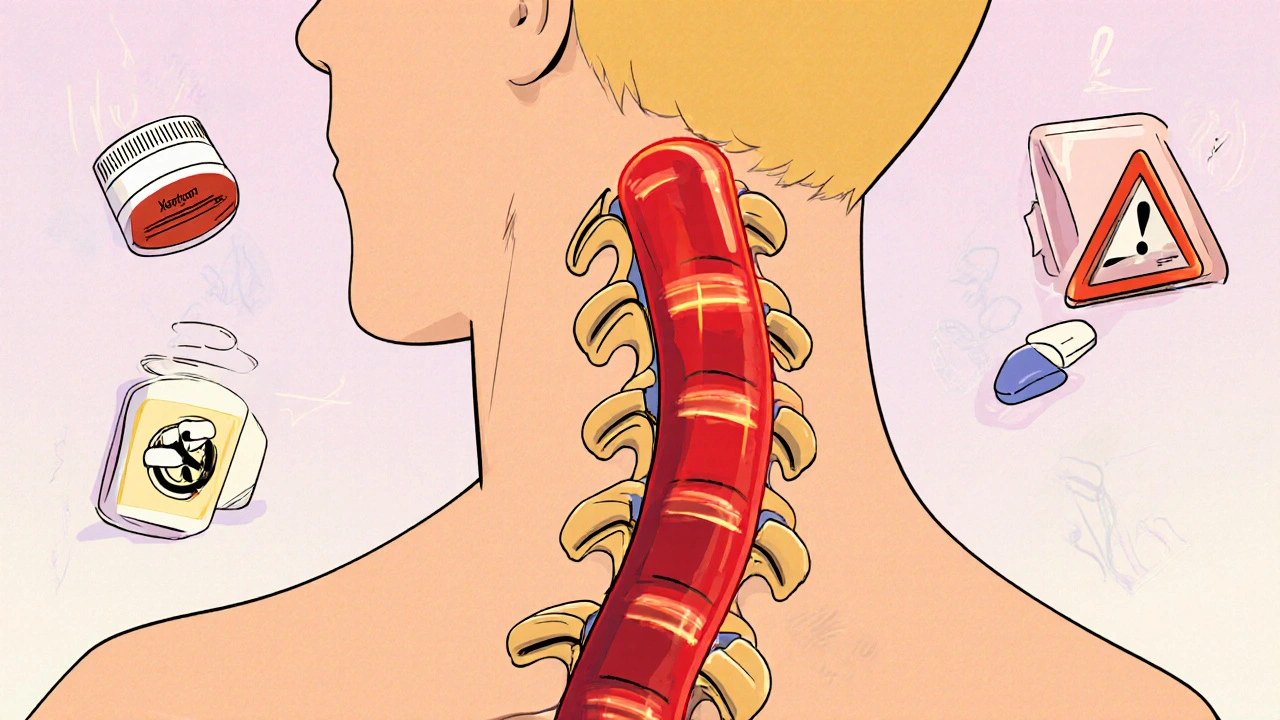
Spinal and epidural procedures on blood thinners carry a small but serious risk of hematoma. Learn the real risks, timing rules for warfarin, LMWH, and DOACs, and how to protect yourself from permanent nerve damage.
- November 10 2025
- Tony Newman
- 11 Comments
