Lupus: What to Watch For and How to Manage It
Lupus is an autoimmune condition where the immune system attacks healthy tissue. That attack can show up in many ways: joint pain, rash, fatigue, fever, or organ problems. Because those signs overlap with other conditions, people often wait months before getting a clear diagnosis.
If you suspect lupus, start by tracking symptoms. Note when fatigue hits, if rashes follow sun exposure, and whether joint pain moves between different joints. Bring this simple log to your doctor — it makes spotting patterns much easier than relying on memory.
How doctors diagnose lupus
There’s no single test that proves lupus. Doctors combine your history, physical exam, blood tests (like ANA, anti-dsDNA, and complement levels), and sometimes urine or imaging studies. A rheumatologist usually leads this workup. If your tests are borderline, repeated checks over weeks or months are common — lupus can declare itself slowly.
Treatments that actually help
Treatment aims to reduce inflammation, prevent flares, and protect organs. Common medicines include hydroxychloroquine for overall control, short courses of corticosteroids for flares, and immunosuppressants (like methotrexate, azathioprine, or mycophenolate) when organs are at risk. Newer biologics are options for people who don’t respond to older drugs.
Medication choice depends on which parts of the body are affected and how severe the disease is. Talk openly with your doctor about side effects and monitoring — regular blood tests are often needed when you’re on immunosuppressants.
Aside from drugs, simple habits make a big difference. Sun protection matters: many people with lupus are photosensitive, so wear a high-SPF sunscreen and long sleeves on sunny days. Sleep, stress management, and gentle exercise (like walking or swimming) help energy and joint pain. Smoking worsens vascular risk and can make some medications less effective — quitting helps.
When a flare hits, act fast. Contact your care team if you get new chest pain, shortness of breath, significant swelling, sudden severe headache, vision changes, or a high fever. For milder flares, an extra rest day, short steroid adjustments (only under guidance), and increased hydration can help until you reach your clinician.
Living with lupus can feel unpredictable, but building a partnership with a rheumatologist, keeping a symptom log, and using practical daily strategies reduces surprises. Support groups — online or local — can offer tips from people who’ve tried different treatments and lifestyle adjustments.
If you want clear, reliable info on specific medications or recent research, ask your doctor for sources or check reputable medical sites. Your care plan should fit your life: don't be afraid to ask questions, request second opinions, or discuss quality-of-life goals with your team.
Lupus and Allergies: What's the Connection?
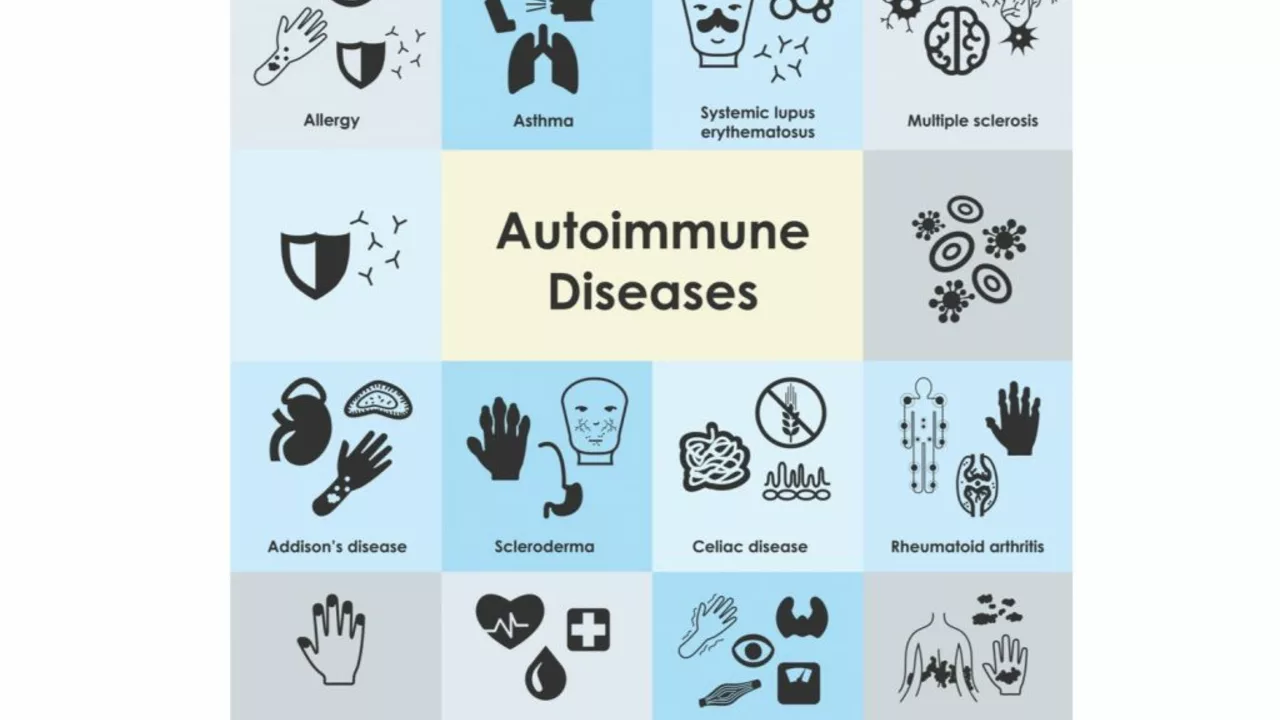
As a lupus patient, I've always wondered about the connection between lupus and allergies. It turns out that lupus, an autoimmune disease, can cause an overactive immune system that may lead to increased allergies. This means that our bodies might react more strongly to allergens, making us more prone to allergic reactions. Moreover, some lupus medications can also cause or worsen allergies. It's essential for those with lupus to be aware of this connection and take necessary precautions to manage their allergies effectively.
- June 18 2023
- Tony Newman
- 15 Comments
The Relationship Between Lupus and Joint Pain
As someone living with lupus, I can attest to the debilitating joint pain it often causes. Lupus is an autoimmune disease that affects various parts of the body, including the joints, leading to inflammation and pain. It's believed that up to 90% of lupus patients experience joint pain, making it one of the most common symptoms of the condition. This pain can range from mild to severe and may affect multiple joints, making everyday tasks difficult. It's crucial to work closely with your healthcare team to manage this pain, as it can greatly impact your quality of life.
- June 2 2023
- Tony Newman
- 9 Comments
