Neuraxial Procedures: What They Are, Why They Matter, and What You Need to Know
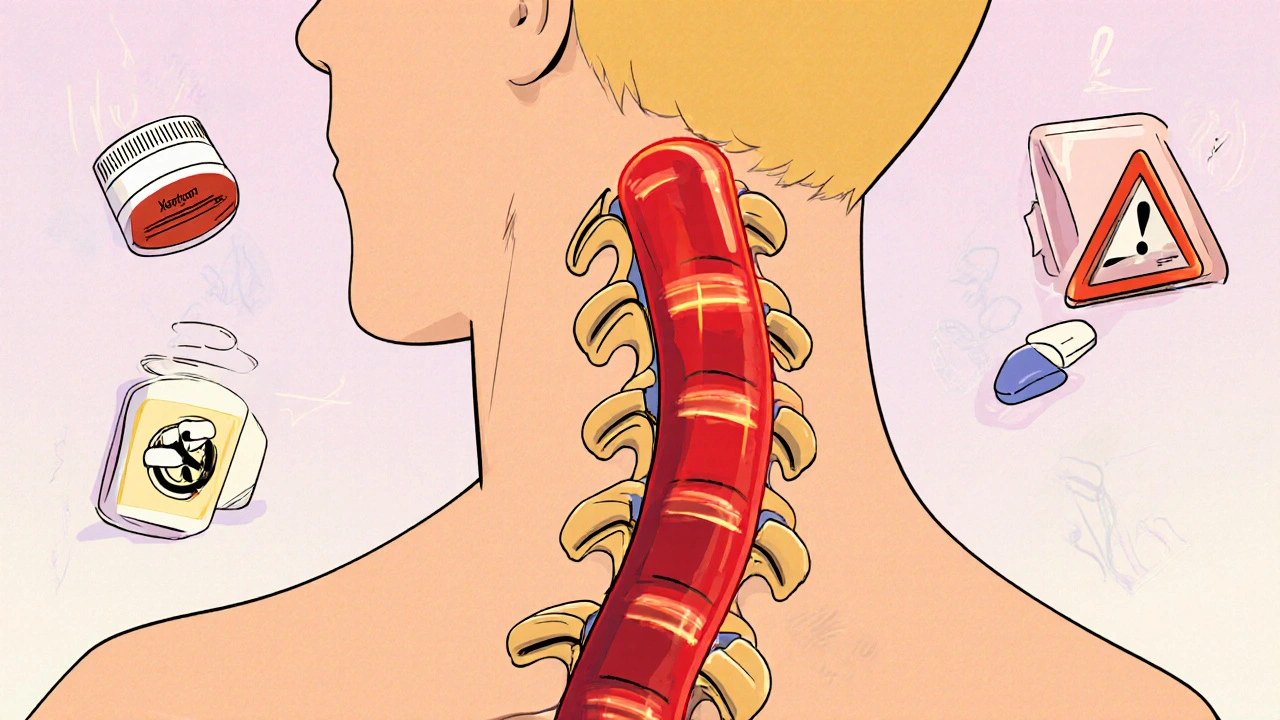
When you hear neuraxial procedures, medical techniques that deliver medication directly to the spinal cord or surrounding nerves to block pain. Also known as regional anesthesia, it isn’t just for surgery—it’s a go-to for childbirth, chronic back pain, and even post-op recovery. These methods let you stay awake while numbing only the part of your body that needs it, avoiding the fog and nausea of full anesthesia. Unlike pills or IV drugs that travel through your whole system, neuraxial techniques target pain at its source, giving you better control with fewer side effects.
Two main types of neuraxial procedures dominate clinical use: spinal anesthesia, a single injection into the fluid around the spinal cord that works fast and lasts a few hours, and epidural anesthesia, a catheter placed just outside that fluid space, allowing continuous or repeated dosing for longer procedures like labor. Both are performed with precision, often guided by real-time feedback from the patient and the doctor’s feel for anatomy. They’re not risky when done right, but they do require skill—you’re not just sticking a needle in your back, you’re navigating a narrow space between delicate tissues. That’s why they’re usually handled by anesthesiologists, not general practitioners.
These procedures connect deeply with other areas of health you might not expect. For example, if you’re managing chronic pain or recovering from surgery, neuraxial techniques can reduce your reliance on opioids, which ties into medication safety and efforts to cut down on polypharmacy. Older adults on multiple drugs often benefit because neuraxial pain control lowers the need for additional pills that could interact badly. Even in pregnancy, where drug choices are limited, epidurals are among the safest and most effective options for pain relief—linking directly to concerns around post-menopausal women and medication changes or pregnancy tremors by offering targeted relief without systemic effects.
But they’re not perfect. Some people get headaches after spinal taps. Others feel temporary numbness or weakness in their legs. Rarely, nerve damage or infection can happen. That’s why knowing the signs of trouble matters—just like you’d watch for side effects from bisoprolol or DPP-4 inhibitors. The goal isn’t to avoid these procedures, but to understand them well enough to ask the right questions: Is this the best option for me? What are the alternatives? How will it affect my other meds?
Below, you’ll find real-world guides that dig into how these procedures fit into broader health strategies—from reducing drug dependence to managing pain without overmedicating. Whether you’re a patient preparing for surgery, a caregiver helping someone through labor, or just someone trying to make sense of medical jargon, these posts give you clear, no-fluff answers.
Epidural and Spinal Procedures on Anticoagulants: What You Need to Know About Hematoma Risks
Spinal and epidural procedures on blood thinners carry a small but serious risk of hematoma. Learn the real risks, timing rules for warfarin, LMWH, and DOACs, and how to protect yourself from permanent nerve damage.
- November 10 2025
- Tony Newman
- 11 Comments
