Obstructive Pulmonary Disease: What You Need to Know
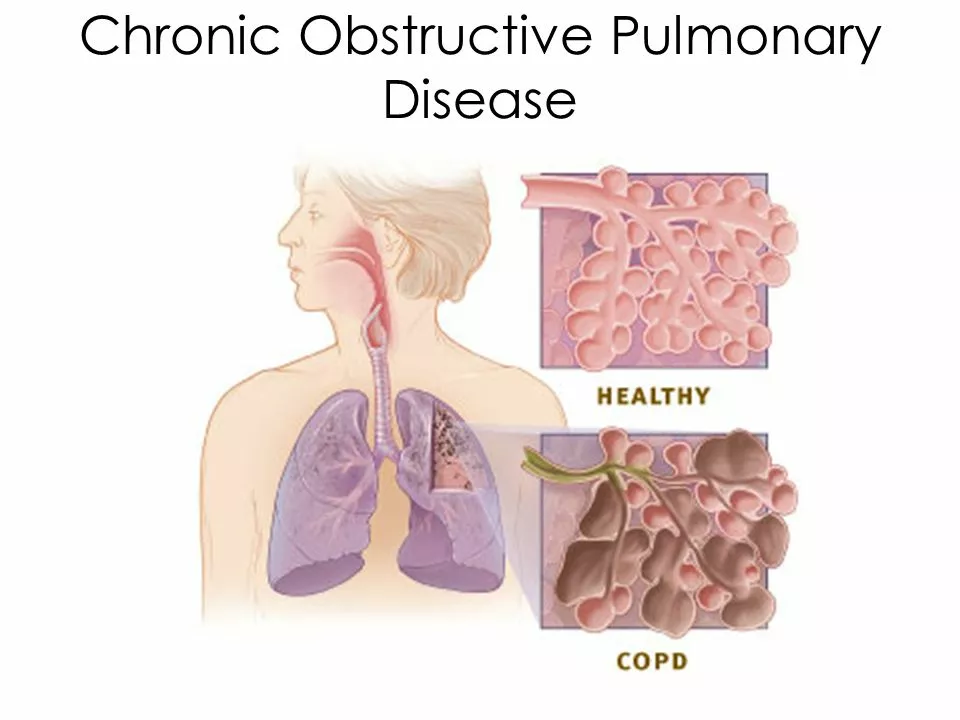
Shortness of breath that slowly gets worse, a cough that won’t quit, and feeling tired after small tasks — those are common signs of obstructive pulmonary disease, often called COPD. If you or someone you care for has trouble breathing during everyday activities, this page gives clear, practical steps you can use right now.
Spotting symptoms and warning signs
Early signs are easy to miss. Watch for persistent cough, sputum that changes color or amount, wheezing, and needing frequent breaks while walking. If you notice fast breathing at rest, blue lips or fingers, confusion, or high fever with increased breathlessness, get urgent medical help.
Doctors confirm COPD with a simple breathing test called spirometry. It measures how much air you can force out and how fast. If you haven’t had this test and symptoms are getting worse, ask your provider for it.
Treatment and everyday management
Medications reduce symptoms and cut flare-ups. Short-acting bronchodilators (like albuterol) give quick relief during breathless moments. Long-acting bronchodilators (LABA or LAMA) work daily to keep airways open. Inhaled steroids help some people who have frequent flare-ups. Many patients use combination inhalers — your doctor will pick what fits you.
Oxygen therapy helps people with low blood oxygen. It’s prescribed after testing. Pulmonary rehab — a short program with exercise, breathing practice, and education — often changes life for the better. If you’ve never tried it, ask your clinic whether a program is available nearby or online.
Small daily habits matter: stop smoking and avoid secondhand smoke, get the yearly flu shot and pneumococcal vaccine, and avoid air pollution when possible. Learn breathing exercises like pursed-lip breathing to slow each breath and reduce panic during flare-ups. Try to stay active within limits — light walking or chair exercises help keep muscles working and reduce breathlessness over time.
Plan ahead for flare-ups. Keep rescue inhalers handy, know how to spot worsening symptoms, and have a written action plan from your provider. If antibiotics or steroids are recommended for flare-ups, ask when to start them.
Need help quitting smoking? Nicotine replacement, varenicline, and counseling work for many people. Talk to a clinician about options and coverage — quitting is the single most effective step to slow COPD progression.
Managing COPD is a team effort. Your doctor, respiratory therapist, pharmacist, and rehab team all have useful roles. Small, consistent changes often give the biggest wins: better sleep, fewer flare-ups, and more confidence with daily tasks.
If you’re unsure what to do next, schedule a visit, ask for spirometry, and request a simple inhaler check so you’re using the device correctly. Clear steps and the right support make breathing easier over time.
The Link Between Obstructive Pulmonary Disease and Asthma
In a recent blog post, I came across some fascinating information about the connection between obstructive pulmonary disease (COPD) and asthma. Both are chronic respiratory conditions that cause breathing difficulties, but they have different causes and treatments. It turns out that some people may have both conditions, which is known as asthma-COPD overlap (ACO), making it challenging to manage and treat their symptoms. Studies have shown that people with ACO experience more frequent exacerbations and a more rapid decline in lung function compared to those with asthma or COPD alone. It's essential to be aware of this link and get a proper diagnosis to ensure the most effective treatment plan for your condition.
- May 20 2023
- Tony Newman
- 20 Comments
