Understanding Obstructive Pulmonary Disease and Asthma
As someone who is passionate about health, I have always been intrigued by how our bodies function, and how various illnesses can affect us. One such topic that has caught my attention recently is the link between Obstructive Pulmonary Disease and Asthma. In this article, I will be sharing my research on these two respiratory conditions and exploring their connection. So, without further ado, let's dive into the subject matter!
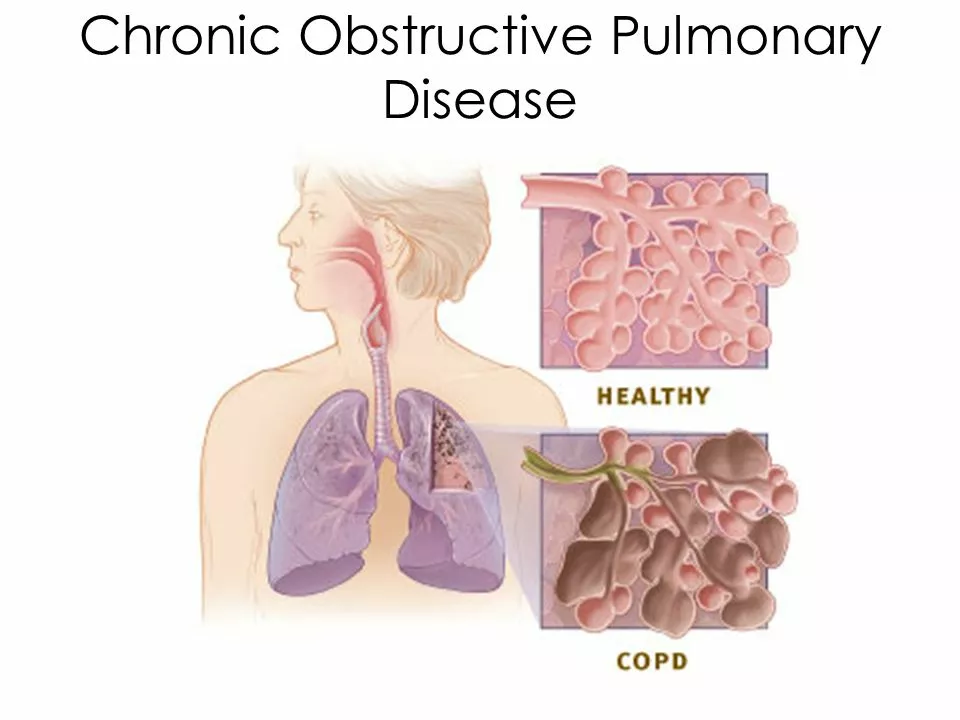
What is Obstructive Pulmonary Disease?
Obstructive Pulmonary Disease (OPD) is a term used to describe a group of lung diseases that limit airflow in the respiratory system. These conditions cause the airways to become narrow, making it difficult for air to flow in and out of the lungs. The most common types of OPD are Chronic Obstructive Pulmonary Disease (COPD) and Asthma. COPD is a progressive, irreversible disease, while Asthma is a reversible condition that can be managed with the right treatment.
What is Asthma?
Asthma is a chronic respiratory condition characterized by episodes of inflammation and narrowing of the airways. It can cause symptoms such as shortness of breath, wheezing, coughing, and chest tightness. People with asthma may experience flare-ups or exacerbations, during which their symptoms become more severe. Asthma is often triggered by environmental factors, such as allergens, irritants, or infections.
How are OPD and Asthma related?
At first glance, it may seem like OPD and Asthma are two completely separate conditions. However, they do share some similarities, which is why they are often grouped together under the umbrella term of Obstructive Pulmonary Disease. Both conditions involve inflammation and narrowing of the airways, and both can cause shortness of breath, wheezing, and coughing. Additionally, both Asthma and COPD can be triggered by environmental factors, such as allergens and irritants.
Overlap Syndrome: Asthma and COPD
There is a condition known as Asthma-COPD Overlap Syndrome (ACOS) in which individuals have features of both asthma and COPD. This overlap can make diagnosis and treatment more challenging, as symptoms and treatment responses may vary. ACOS is typically diagnosed when a person with chronic respiratory symptoms has a history of both asthma and smoking, the primary risk factor for COPD.
Diagnosing Obstructive Pulmonary Disease and Asthma
Diagnosing OPD and Asthma can be challenging, as their symptoms can be similar and sometimes overlap. A thorough medical history, physical examination, and various tests can help differentiate between the two conditions. Spirometry, a lung function test that measures airflow, is often used to diagnose both Asthma and COPD. However, in Asthma, the results may improve significantly after using a bronchodilator, while in COPD, the improvement may be minimal.
Treatment Options for Obstructive Pulmonary Disease and Asthma
Treatment for OPD and Asthma is focused on managing symptoms, preventing flare-ups, and improving overall lung function. For Asthma, this may involve the use of inhaled corticosteroids, bronchodilators, and allergen avoidance. In COPD, treatment may include bronchodilators, inhaled corticosteroids, and pulmonary rehabilitation. It's important to remember that while Asthma can be well-managed with the right treatment plan, COPD is a progressive disease with no cure.
Preventing Obstructive Pulmonary Disease and Asthma
While the exact causes of OPD and Asthma are not entirely understood, there are steps you can take to reduce your risk of developing these conditions. For starters, avoid smoking and exposure to secondhand smoke, as these are significant risk factors for COPD. Additionally, maintaining a healthy lifestyle, including regular exercise and a balanced diet, can help maintain overall lung health. For those with Asthma, identifying and avoiding triggers is crucial to preventing flare-ups.
Conclusion
In conclusion, Obstructive Pulmonary Disease and Asthma are two respiratory conditions that share some similarities but differ in their progression and treatment. Understanding the link between these diseases is essential for proper diagnosis and management. By staying informed and taking preventive measures, we can work towards better lung health and improved quality of life for those affected by these conditions. I hope this article has provided valuable insight into the link between Obstructive Pulmonary Disease and Asthma, and I encourage you to continue learning and advocating for better respiratory health!

Poorni Joth
May 20, 2023 AT 23:13People should stop ignoring the dieally link between smoking and lung disease!
Yareli Gonzalez
May 22, 2023 AT 12:06It’s great that you’re digging into the overlap between asthma and COPD. Understanding the nuances can really empower patients to manage their symptoms better. Keep sharing these insights, they’re valuable for the community.
Alisa Hayes
May 24, 2023 AT 01:03Great overview of the similarities and differences, especially the part about spirometry results. I appreciate the clear explanation of reversible versus irreversible airway obstruction. The mention of environmental triggers ties everything together nicely. It might also help to include a brief note on the role of genetics in asthma. Overall, a solid summary.
Mariana L Figueroa
May 25, 2023 AT 14:00Learning about the overlap syndrome can be eye opening. It shows why personalized treatment plans are essential. Always talk to your doctor about your specific triggers.
mausumi priyadarshini
May 27, 2023 AT 02:56Honestly, the article seems to oversimplify, however, it does raise some points, which are worth noting, especially the claim that all smokers develop COPD, which is not universally true, and the suggestion that asthma is always reversible, which can be misleading, given the variability among patients.
Carl Mitchel
May 28, 2023 AT 15:53While the enthusiasm is commendable, the reality is that many patients neglect the moral responsibility to quit smoking, which is the single biggest preventable cause of COPD. It’s not enough to just mention lifestyle changes; we must demand stricter public health policies. Moreover, the medical community should stop treating asthma as a trivial condition and recognize its potential severity. Ignoring these facts does a disservice to those suffering.
Suzette Muller
May 30, 2023 AT 04:50Thanks for summarizing the diagnostic tools; spirometry really is the cornerstone. I’d add that bronchodilator response thresholds can vary. It’s also helpful to consider patient history in ambiguous cases.
Josh SEBRING
May 31, 2023 AT 17:46Sure, but the article completely ignores the cost barriers many patients face when accessing spirometry, which is a major oversight. Also, not every clinic has the equipment, so that point feels a bit naive.
Lily Tung
June 2, 2023 AT 06:43Asthma and COPD share many clinical features, yet they differ fundamentally in pathophysiology. Asthma is primarily an inflammatory disorder that responds well to corticosteroids. COPD, on the other hand, involves permanent airway remodeling and loss of elastic recoil. Both conditions can cause wheezing and shortness of breath. The diagnostic process often begins with a careful history of symptoms. Spirometry remains the gold standard for assessing airflow limitation. Reversibility testing helps to distinguish asthma from COPD. In asthma, bronchodilator use leads to a marked improvement in FEV1. In COPD the improvement is modest at best. Treatment strategies must be tailored to the underlying disease. Inhaled corticosteroids are mainstay therapy for persistent asthma. Long‑acting bronchodilators are essential for COPD management. Smoking cessation is the single most important intervention for COPD patients. Vaccinations can reduce exacerbation rates in both diseases. Ongoing research aims to better define the overlap syndrome and improve patient outcomes.
Taryn Bader
June 3, 2023 AT 19:40This really hits home for anyone who has struggled with breathlessness. The tone is both hopeful and realistic.
Myra Aguirre
June 5, 2023 AT 08:36I noticed the article mentions diet but doesn’t go into detail. Nutrition can affect inflammation in the lungs. It might be worth adding a short section on that.
Shawn Towner
June 6, 2023 AT 21:33While adding diet tips sounds nice, the evidence is still weak and many patients focus on medication instead.
Edwin Levita
June 8, 2023 AT 10:30Honestly the piece feels like it’s trying to be dramatic without delivering new data. It repeats what most textbooks already say. I was hoping for fresh perspectives on the overlap syndrome. Perhaps a deeper dive into biomarkers would have helped.
Xander Laframboise
June 9, 2023 AT 23:26I disagree with the claim that the article adds nothing new. It actually compiles recent studies that many clinicians miss. The discussion on eosinophilic phenotypes in COPD is quite relevant. Still, a more thorough analysis of longitudinal outcomes would be beneficial.
Jason Petersen
June 11, 2023 AT 12:23The article is okay but it skips the socioeconomic factors that affect treatment adherence. That’s a major blind spot. Future revisions should address that.
Melissa Gerard
June 13, 2023 AT 01:20Well, if you think it’s that simple, maybe you’re just lazy about digging deeper 😊. The author's focus was on clinical aspects, not a sociological essay.
Cindy Knox
June 14, 2023 AT 14:16Wow, what a heartfelt summary! It really captures the struggle and hope of living with chronic lung disease. I feel inspired to share this with my support group. Keep up the great work!
beverly judge
June 16, 2023 AT 03:13Thank you for the kind words. I would suggest adding a reference to the latest GOLD guidelines for completeness. Also, a brief note on pulmonary rehabilitation could strengthen the conclusion.
Capt Jack Sparrow
June 17, 2023 AT 16:10Look, the facts are clear: asthma and COPD have distinct mechanisms, and you need to treat them accordingly. Don’t mix them up just because they both cause cough. Tailor the meds to the diagnosis.
Manju priya
June 19, 2023 AT 05:06Dear readers, I commend the thoroughness of this article and encourage continued education on respiratory health. It is imperative that we disseminate accurate information to empower patients. Let us strive together for better lung health 😊.