Risk factors: what they mean and how to lower them
Risk factors are anything that makes a health problem more likely to happen. Some you can’t change, like age or family history. Others you can change, like smoking, diet, activity level, or alcohol use. The point is not to scare you—it's to give you clear, usable steps so you can lower your chances of getting sick.
Types of risk factors — quick breakdown
Non-modifiable: age, genetic history, sex, and past medical events. You can’t edit these, but knowing them helps your doctor choose the right tests and treatments.
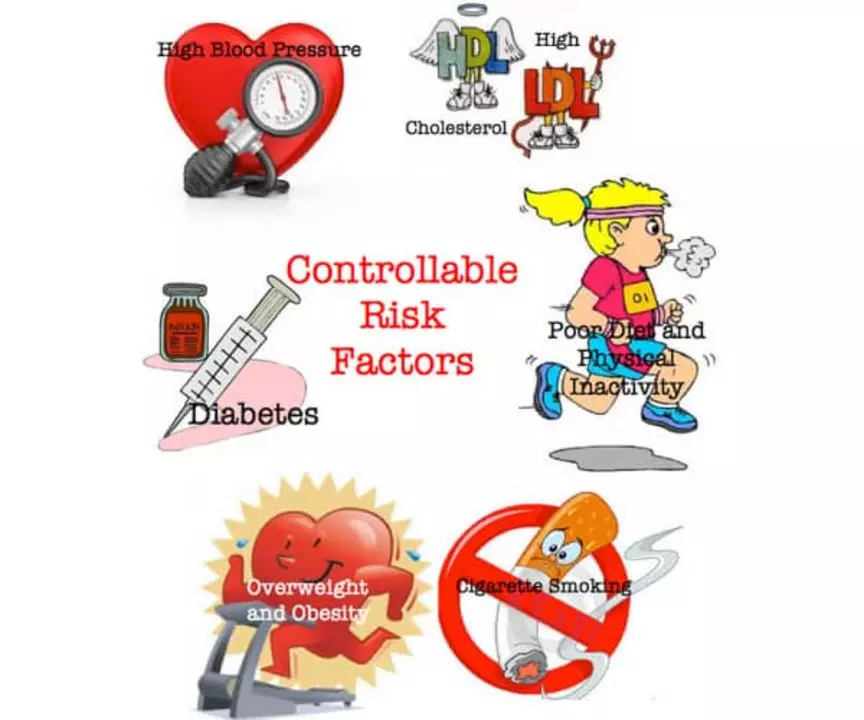
Modifiable: smoking, high blood pressure, high blood sugar, obesity, poor sleep, stress, and some medication choices. These are where most of your power lies. Small changes here often give the biggest payoff.
Practical steps to lower your risk
Get basic checks regularly: blood pressure, fasting blood sugar, cholesterol, BMI. These numbers tell a clear story—if one is off, you can act before symptoms show. Many clinics offer simple risk calculators for heart disease or diabetes; ask your provider to run one for you.
Move more. You don’t need daily marathon training. Aim for 150 minutes a week of moderate activity or short daily walks. Physical activity lowers blood pressure, improves blood sugar, helps mood, and reduces inflammation.
Fix the easy diet wins: cut sugary drinks, add more vegetables, swap processed snacks for whole foods, and watch portion sizes. Changing one habit at a time—like replacing soda with water—stays doable and lasts longer.
Quit smoking and cut back on heavy drinking. Both raise risks for heart disease, some cancers, and infections. If quitting feels overwhelming, ask a doctor about stepwise help: nicotine replacement, medications, or counseling work better than going it alone.
Mind your meds and supplements. Some drugs interact or raise risk for side effects. If you’re taking acid reflux meds, antidepressants, or antifungals, check in with your provider about long-term safety and alternatives. Our site has guides on heartburn drugs, antidepressant choices, and antifungal treatments that can help you get the facts before you talk to a clinician.
Manage stress and sleep. Chronic stress and poor sleep raise inflammation and can make blood sugar and blood pressure harder to control. Simple habits—fixed sleep hours, short relaxation routines, and setting daily priorities—make a real difference.
Know warning signs and act early. If you have a family history of disease, or live with diabetes or mood disorders, schedule regular follow-ups. Early treatment usually means simpler care and better outcomes.
Finally, use trusted resources. Not every online article is accurate. Look for clear, up-to-date info and ask questions during appointments. If you want practical articles tied to specific risks—like diabetes treatments, heartburn options, or managing depression and eating disorders—check the related posts on this site for deeper, user-friendly guides.
Small, steady changes beat dramatic but short-lived fixes. Pick one thing you can improve this week—drink more water, add a 20-minute walk, or book a blood test—and build from there.
How Smoking Increases the Risk of Skin Yeast Infections

Explore how smoking weakens immunity and skin barriers, raising the risk of cutaneous yeast infections, and learn prevention, treatment, and quitting tips.
- October 10 2025
- Tony Newman
- 12 Comments
The Connection between Arrhythmias and Stroke
As a blogger, I've recently come across an interesting topic that I'd like to share with you - the connection between arrhythmias and stroke. Arrhythmias are irregular heartbeats, which can disrupt the normal flow of blood and potentially lead to blood clots. These clots can then travel to the brain and cause a stroke, which can be life-threatening. It's crucial to be aware of this connection and monitor any heart-related issues, as managing arrhythmias can help prevent strokes. Remember, staying informed and taking care of your heart can go a long way in ensuring your overall health.
- May 11 2023
- Tony Newman
- 17 Comments
