Spinal Anesthesia: What It Is, How It Works, and What to Expect
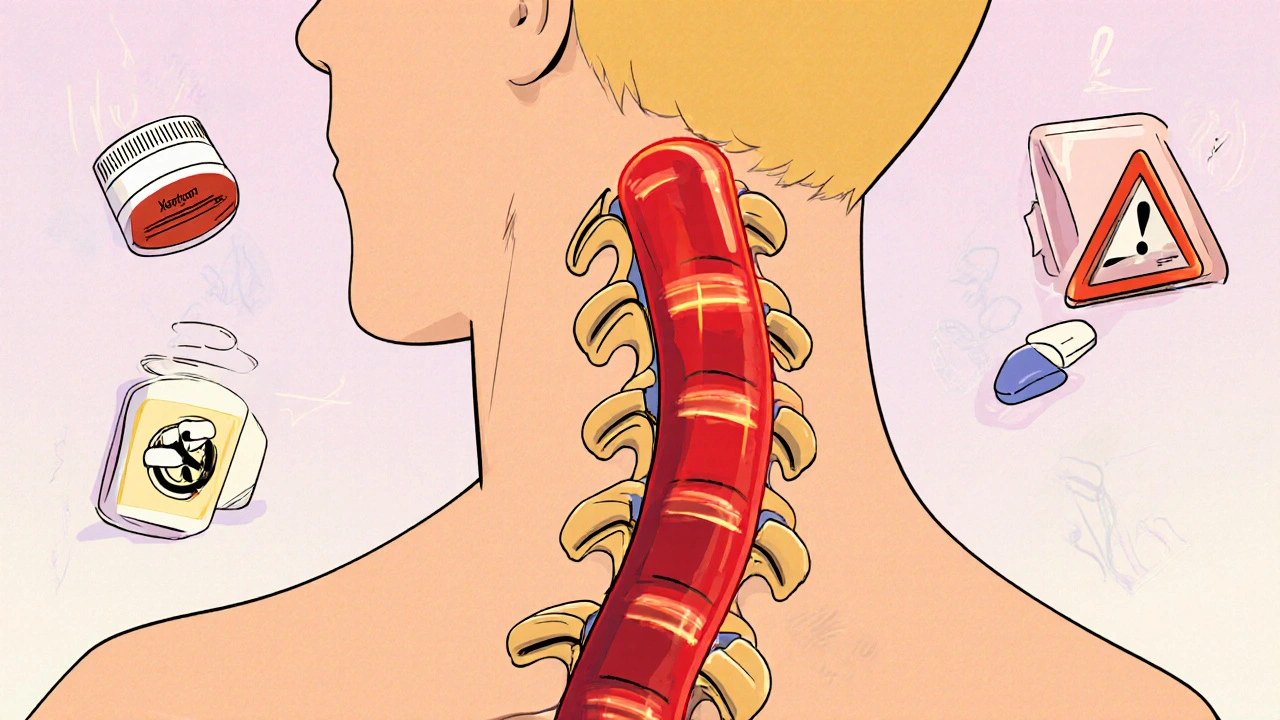
When you need surgery on your lower body—like a C-section, hip replacement, or hernia repair—you might hear your doctor mention spinal anesthesia, a type of regional anesthesia that blocks pain signals from the lower half of your body by injecting numbing medicine into the fluid around your spinal cord. Also known as subarachnoid block, it’s fast-acting, highly effective, and often preferred over general anesthesia for certain procedures because it avoids putting you fully to sleep. Unlike general anesthesia, which affects your whole body and brain, spinal anesthesia lets you stay awake and aware while keeping you completely pain-free below the injection site.
It works by targeting the nerves that carry pain signals from your legs, abdomen, and pelvis up to your brain. A thin needle is inserted between two bones in your lower back, and a small amount of local anesthetic—like bupivacaine or lidocaine—is delivered directly into the cerebrospinal fluid. Within minutes, you’ll feel numbness starting in your toes and moving upward. The effect usually lasts 1 to 3 hours, depending on the drug and dose. You might also get a mild sedative to help you relax, but you won’t be unconscious. This makes spinal anesthesia a smart choice for many patients, especially those with breathing issues or higher risks from being put to sleep.
Spinal anesthesia is closely related to epidural anesthesia, a similar technique where medicine is injected just outside the spinal sac, often used for labor pain or longer procedures. While both block pain in the lower body, spinal anesthesia works faster and uses less medication, but it’s usually a one-time dose. Epidurals can be left in place with a catheter for continuous pain control. Knowing the difference helps you ask better questions and understand your options. Common side effects include low blood pressure, headaches (from fluid leakage), and temporary difficulty urinating. Serious complications like nerve damage or infection are rare but possible. Your anesthesiologist will check your health history, especially for blood thinners, spine issues, or allergies, before deciding if it’s right for you.
Spinal anesthesia isn’t just for hospitals. It’s also used in outpatient clinics and even some pain management centers for chronic conditions like severe back pain or reflex sympathetic dystrophy. It’s a powerful tool in pain management, a field focused on reducing suffering without relying on opioids or long-term drugs. Many people find it gives them relief without the drowsiness or addiction risks tied to oral painkillers. Whether you’re preparing for surgery or exploring alternatives to strong medications, understanding how spinal anesthesia works helps you take control of your care.
Below, you’ll find real-world guides from people who’ve gone through it—what to expect before, during, and after. Some share how they managed side effects like headaches or shaking. Others explain how they talked to their doctors about risks, especially if they were on blood thinners or had prior back surgery. You’ll also see how it compares to other types of anesthesia, and what lifestyle steps you can take afterward to recover faster and avoid complications.
Epidural and Spinal Procedures on Anticoagulants: What You Need to Know About Hematoma Risks
Spinal and epidural procedures on blood thinners carry a small but serious risk of hematoma. Learn the real risks, timing rules for warfarin, LMWH, and DOACs, and how to protect yourself from permanent nerve damage.
- November 10 2025
- Tony Newman
- 11 Comments
