For years, gout was seen as a painful but inevitable condition-something you just had to live with. But today, we know better. Gout isn’t just about flare-ups; it’s a metabolic disease driven by high levels of uric acid in the blood. And if you keep that level too high, crystals form in your joints, leading to inflammation, damage, and even tophi-those visible lumps under the skin. The good news? You can stop it. The key is urate targets.
What Exactly Is a Urate Target?
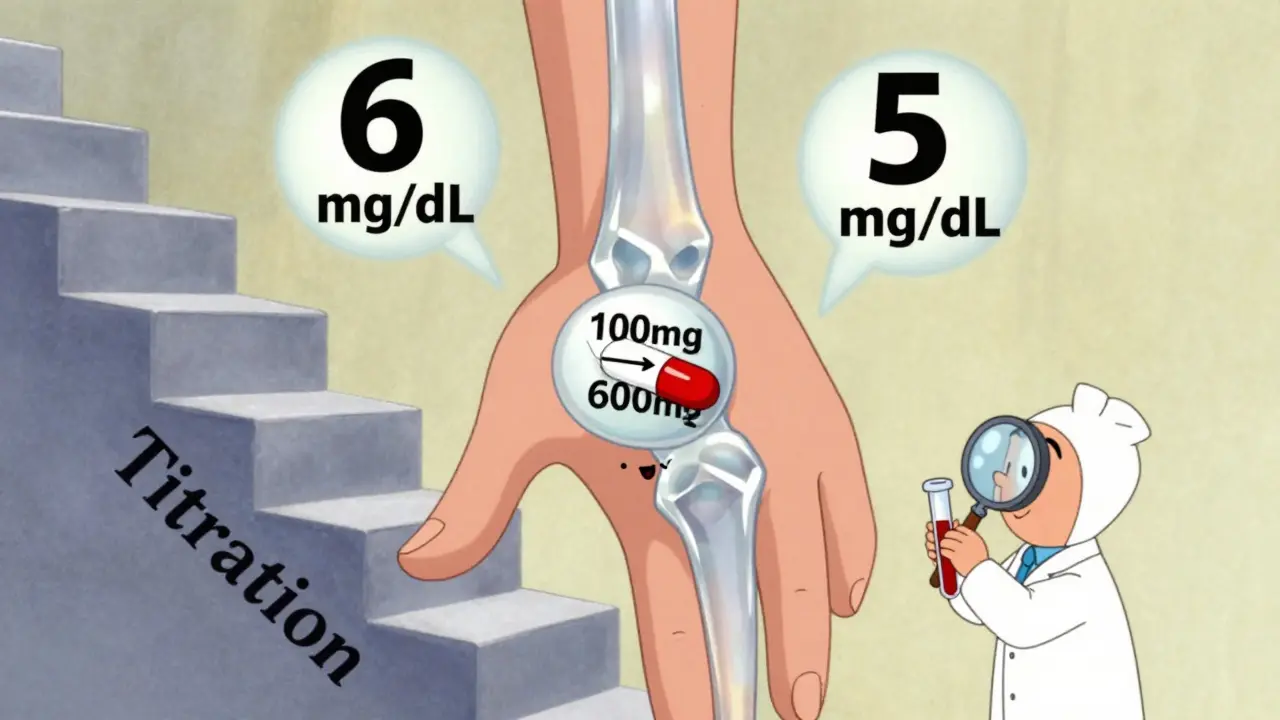
A urate target is the specific level of uric acid you need to reach in your blood to prevent gout from getting worse. It’s not a suggestion. It’s a medical goal. The science is clear: when serum urate drops below 6 mg/dL (or 360 micromol/L), your body starts dissolving the crystals that cause pain. That’s the magic number. For most people with gout, staying under this level cuts flare-ups by more than 70%.
But if you have severe gout-with tophi, joint damage, or frequent flares-your target should be even lower: under 5 mg/dL (300 micromol/L). Why? Because dissolving larger crystal deposits takes more time and more aggressive control. Studies show that patients hitting this lower target lose up to 89% of their tophi burden over time, compared to just 72% when staying at 6 mg/dL.
And here’s something most people don’t know: you don’t want to go too low. Below 3 mg/dL, there’s no extra benefit, and it might even cause problems. So the goal isn’t to crush uric acid-it’s to hold it in the sweet spot where crystals dissolve but your body stays balanced.
Allopurinol: The First-Line Workhorse
Allopurinol has been the go-to drug for gout for over 60 years. It works by blocking the enzyme that makes uric acid. Simple. Effective. Cheap. Generic versions cost between $4 and $12 a month in the U.S., making it accessible to nearly everyone.
But here’s the catch: most people start too low and never adjust. Doctors often begin with 100 mg/day, sometimes even 50 mg/day if kidney function is reduced. That’s fine for a trial-but if your uric acid doesn’t drop below 6 mg/dL after a few months, you’re not getting the benefit.
Real-world data shows that 30-50% of patients need more than 300 mg/day to reach their target. Some need 600 mg, even 800 mg. And yes, that’s safe-if you monitor it. The key is monthly blood tests. Every 4 to 6 weeks, check your uric acid level and increase the dose by 50-100 mg until you hit your target. This isn’t guesswork. It’s science.
One study found that patients who had monthly uric acid checks were 31% more likely to reach their target than those checked only every three months. Yet, only 54% of Medicare patients get those monthly tests. That’s a huge gap between what we know works and what actually happens.

Febuxostat: The Alternative for Tough Cases
Febuxostat is newer, pricier (around $30-$50/month), and works differently. It also blocks uric acid production but is more potent, especially in people with kidney disease. A 2023 meta-analysis found it achieves target levels in 15% more patients with severe CKD than allopurinol.
That makes it a strong option if you have stage 3 or higher chronic kidney disease, or if allopurinol didn’t work even at high doses. It starts at 40 mg/day and can be bumped up to 80 mg if needed. Unlike allopurinol, you don’t need to adjust the dose based on kidney function-making it simpler for some patients.
But it’s not without risks. The FDA requires a black box warning for possible heart-related death, though the actual risk is small and mostly seen in people with existing heart disease. For most patients without cardiovascular issues, febuxostat is a safe and effective alternative.
Guidelines differ slightly here. The American College of Rheumatology (ACR) says allopurinol should be first, no matter your kidney health. NICE (UK) and EULAR (Europe) say either drug is fine as long as you pick based on your health and preference. In practice, that means your doctor should talk to you-not just prescribe by default.
Why Most People Fail to Reach Their Target
Here’s the uncomfortable truth: even with these two powerful drugs, only about 42% of gout patients hit their urate target within a year. Why?
- Dosing too low: Many doctors start with 100 mg allopurinol and never go higher. That’s like trying to put out a house fire with a water bottle.
- No monitoring: If you don’t test your uric acid, you don’t know if the drug is working. Blood tests aren’t optional-they’re essential.
- Fear of side effects: About 68% of patients stop or refuse to increase their dose because they’re scared of reactions. Allopurinol hypersensitivity syndrome is rare (0.1-0.4%), but it’s serious. If you’re of Asian descent or have the HLA-B*5801 gene, testing before starting helps avoid this.
- The flare paradox: When you start lowering uric acid fast, crystals can shift and trigger flares. This isn’t the drug failing-it’s the disease reacting. Doctors should start with low-dose colchicine or NSAIDs during the first 6 months to prevent this.
Patients often say they waited over six months to feel better. Some needed doses over 400 mg. And 62% blamed their doctors for not explaining how titration works. Education matters as much as medication.
The New Frontiers: Precision and Dissolution
Science is moving beyond one-size-fits-all. In 2024, the GOUT-PRO study showed that using genetic testing to guide allopurinol dosing-looking at ABCG2 and SLC22A12 gene variants-boosted target achievement from 61% to 83% in just six months. That’s a game-changer.
Another breakthrough? The idea of “treat-to-dissolve.” Instead of just aiming for 5 mg/dL, some experts now want proof that crystals are gone. Dual-energy CT scans can show urate deposits. If those are gone, you might be able to relax your target. This isn’t standard yet-but it’s coming.
Meanwhile, new drugs like verinurad are in trials. They work differently, helping the kidneys flush out uric acid instead of blocking its production. They could mean fewer pills, fewer dose jumps, and better results.
What You Need to Do Right Now
If you have gout and are on medication:
- Ask for a serum uric acid test. Don’t wait for symptoms.
- If your level is above 6 mg/dL, ask if your dose can be increased.
- If you’re on allopurinol and still having flares, don’t assume it’s not working. Ask about doubling or tripling the dose.
- If you have kidney disease, ask if febuxostat might be better for you.
- Ask about starting low-dose colchicine for the first 6 months to prevent flares.
- Get genetic testing if you’re of Asian descent or have had unexplained rashes with allopurinol.
Gout is no longer a life sentence. It’s a chronic condition you can control-with the right target, the right drug, and the right monitoring. You don’t need to live with pain. You just need to take the next step.
What is the ideal urate target for gout?
For most people with gout, the target is below 6 mg/dL (360 micromol/L). If you have tophi, joint damage, or frequent flares, aim for below 5 mg/dL (300 micromol/L). Going below 3 mg/dL offers no extra benefit and may cause harm.
Is allopurinol better than febuxostat?
Allopurinol is cheaper and works well for most people, especially if dosed correctly. Febuxostat is more effective in people with severe kidney disease and may be better if allopurinol doesn’t work or causes side effects. Neither is universally better-it depends on your health, kidney function, and cost.
Why do I still get flares after starting urate-lowering therapy?
When uric acid drops quickly, crystals can break loose and trigger inflammation. This is called the "flare paradox." It’s not the drug failing-it’s your body adjusting. Taking low-dose colchicine or an NSAID for the first 6 months can prevent these flares.
How often should I get my uric acid tested?
Every 4 to 6 weeks while adjusting your dose. Once you hit your target and stay there for 3-6 months, you can reduce testing to every 6 months. Monthly checks during titration improve success rates by 31%.
Can I stop taking medication if I feel fine?
No. Gout is not cured by feeling better. If you stop, uric acid rises again, crystals reform, and damage returns. Urate-lowering therapy is lifelong for most people-like taking blood pressure medication. You don’t stop because you feel fine-you stop because your doctor says it’s safe.
Is genetic testing for allopurinol necessary?
Not for everyone. But if you’re of Asian descent, have had a rash with allopurinol before, or have a family history of severe reactions, testing for HLA-B*5801 can prevent life-threatening hypersensitivity. It’s a simple blood test and worth considering.